- What are ideal blood sugar levels for preventing repeat strokes, heart attacks?
- Understanding Blood Sugar and Cardiovascular Health
- Optimal Blood Sugar Levels
- Mechanisms Linking Blood Sugar and Cardiovascular Events
- Current Guidelines and Recommendations
- Management Strategies
- Monitoring and Follow-Up
- Importance of Comprehensive Cardiovascular Risk Management
- Special Considerations in Specific Populations
- Future Directions and Research
- Conclusion
- References
What are ideal blood sugar levels for preventing repeat strokes, heart attacks?
Blood sugar levels play a crucial role in the overall health of individuals, particularly those who have already experienced cardiovascular events such as strokes and heart attacks. Maintaining optimal blood sugar levels is essential in preventing recurrent incidents and promoting cardiovascular health. This article delves into the ideal blood sugar levels for preventing repeat strokes and heart attacks, exploring the physiological mechanisms, current guidelines, and management strategies supported by research.
Understanding Blood Sugar and Cardiovascular Health
Blood sugar, or glucose, is the primary source of energy for the body’s cells. It is regulated by insulin, a hormone produced by the pancreas. When blood sugar levels are too high (hyperglycemia) or too low (hypoglycemia), it can lead to serious health complications, including cardiovascular diseases.
High blood sugar levels can cause damage to blood vessels and nerves that control the heart. Over time, this damage can lead to the buildup of plaques in arteries, a condition known as atherosclerosis, which increases the risk of strokes and heart attacks. Conversely, low blood sugar levels can cause symptoms such as dizziness, confusion, and in severe cases, loss of consciousness, which can also indirectly increase cardiovascular risk.
Optimal Blood Sugar Levels
General Population vs. High-Risk Individuals
For the general population, the American Diabetes Association (ADA) recommends the following blood sugar targets:
– Fasting Blood Sugar: 80-130 mg/dL
– Postprandial Blood Sugar (1-2 hours after meals): Less than 180 mg/dL
– HbA1c (Glycated Hemoglobin): Less than 7%
However, for individuals who have experienced a stroke or heart attack, these targets may need to be more stringent to prevent recurrence. The International Diabetes Federation (IDF) and other health organizations often advocate for lower targets in high-risk individuals to reduce the risk of further cardiovascular events.
Research Findings
A systematic review published in the journal “Diabetes Care” indicated that maintaining HbA1c levels below 6.5% could significantly reduce the risk of recurrent cardiovascular events in diabetic patients with a history of stroke or heart attack (Zoungas et al., 2014). Similarly, the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial demonstrated that intensive glucose control (targeting an HbA1c below 6.0%) could reduce the risk of nonfatal myocardial infarction, although it did not significantly affect stroke rates (Gerstein et al., 2008).
Mechanisms Linking Blood Sugar and Cardiovascular Events
Endothelial Dysfunction
High blood sugar levels cause endothelial dysfunction, which is the impaired functioning of the inner lining of blood vessels. This dysfunction is a precursor to atherosclerosis and thrombosis, both of which are critical in the development of strokes and heart attacks. Hyperglycemia induces oxidative stress and inflammation, leading to the production of reactive oxygen species (ROS) that damage endothelial cells (Forbes & Cooper, 2013).
Platelet Aggregation
Elevated blood sugar levels increase platelet aggregation and adhesion, which promotes the formation of clots. This hypercoagulable state is particularly dangerous for individuals with pre-existing cardiovascular conditions as it can trigger thrombotic events leading to heart attacks or strokes (Davi et al., 2005).
Current Guidelines and Recommendations
American Diabetes Association (ADA)
The ADA emphasizes individualized treatment goals for blood sugar management in high-risk patients. For those with cardiovascular disease, the ADA suggests more stringent HbA1c targets, typically below 7%, but acknowledges that targets as low as 6.5% might be appropriate for some individuals without significant risk of hypoglycemia (American Diabetes Association, 2020).
American Heart Association (AHA)
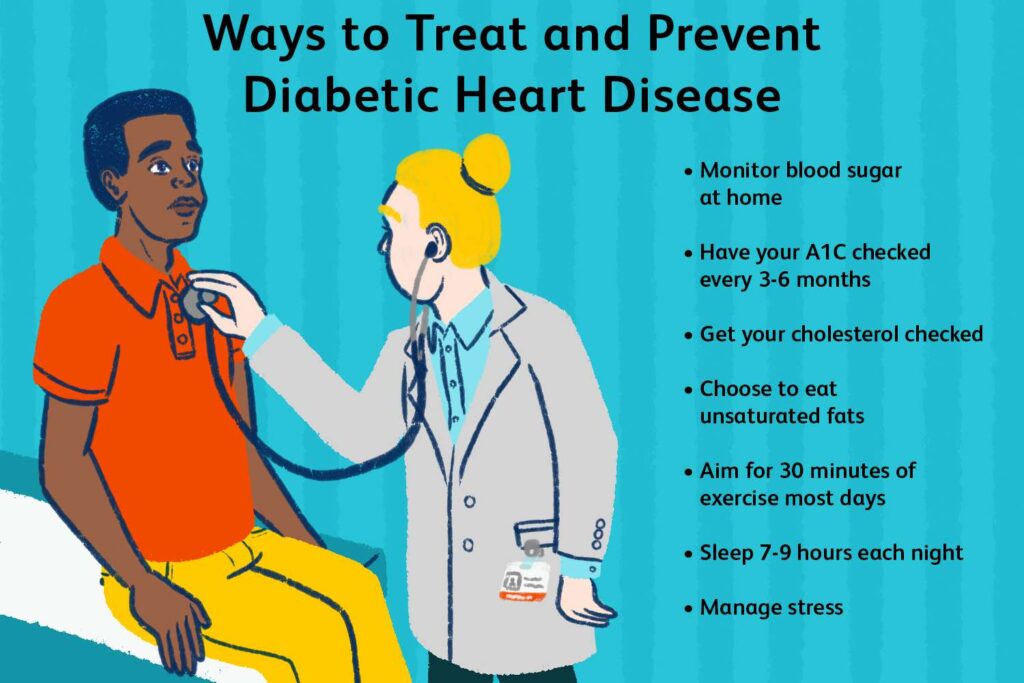
The AHA recommends comprehensive cardiovascular risk management, which includes controlling blood sugar levels, maintaining a healthy diet, engaging in regular physical activity, and adhering to prescribed medications. The AHA suggests that blood sugar levels should be managed aggressively in patients with a history of cardiovascular events to prevent recurrence (American Heart Association, 2020).
Management Strategies
Lifestyle Modifications
1. Diet: Adopting a heart-healthy diet that is low in refined sugars and high in fiber can help maintain optimal blood sugar levels. The Mediterranean diet, rich in fruits, vegetables, whole grains, and healthy fats, has been shown to improve glycemic control and reduce cardiovascular risk (Estruch et al., 2018).
2. Exercise: Regular physical activity enhances insulin sensitivity and helps in maintaining blood sugar levels within the target range. The ADA recommends at least 150 minutes of moderate-intensity aerobic exercise per week for individuals with diabetes (American Diabetes Association, 2020).
3. Weight Management: Maintaining a healthy weight through diet and exercise can significantly improve blood sugar control and reduce the risk of recurrent cardiovascular events. Even a modest weight loss of 5-10% can have substantial benefits (Wing et al., 2011).
Pharmacological Interventions
1. Antihyperglycemic Agents: Several classes of medications, including metformin, sulfonylureas, DPP-4 inhibitors, GLP-1 receptor agonists, and SGLT2 inhibitors, are used to manage blood sugar levels. The choice of medication depends on individual patient characteristics and comorbidities.
2. Cardioprotective Drugs: In addition to antihyperglycemic agents, patients with a history of cardiovascular events are often prescribed medications that directly reduce cardiovascular risk, such as statins, antihypertensives, and antiplatelet agents. Some antihyperglycemic drugs, like SGLT2 inhibitors (e.g., empagliflozin) and GLP-1 receptor agonists (e.g., liraglutide), have shown cardiovascular benefits beyond glucose control (Marso et al., 2016; Zinman et al., 2015).
3. Insulin Therapy: In cases where oral medications are insufficient to achieve target blood sugar levels, insulin therapy may be necessary. Insulin regimens are tailored to individual needs, balancing the goals of tight glucose control with the risk of hypoglycemia.
Monitoring and Follow-Up
Continuous monitoring of blood sugar levels is crucial for individuals at high risk of recurrent cardiovascular events. Self-monitoring of blood glucose (SMBG) helps patients track their blood sugar levels and make informed decisions about diet, exercise, and medication. Additionally, regular follow-up appointments with healthcare providers are essential to assess the effectiveness of the management plan and make necessary adjustments.
Importance of Comprehensive Cardiovascular Risk Management
Managing blood sugar levels is only one aspect of comprehensive cardiovascular risk management. Patients with a history of stroke or heart attack must also address other modifiable risk factors, such as hypertension, dyslipidemia, smoking, and obesity, to reduce their overall risk of recurrent cardiovascular events.
Blood Pressure Control
Hypertension is a significant risk factor for both strokes and heart attacks. According to the American Heart Association, blood pressure should be kept below 130/80 mmHg in individuals with a history of cardiovascular disease (American Heart Association, 2020). Antihypertensive medications, such as ACE inhibitors, ARBs, beta-blockers, and calcium channel blockers, are commonly used to achieve these targets.
Lipid Management
Dyslipidemia, characterized by elevated levels of LDL cholesterol and low levels of HDL cholesterol, is another critical risk factor. Statins are the cornerstone of lipid-lowering therapy and have been shown to reduce the risk of recurrent cardiovascular events. In some cases, additional lipid-lowering agents, such as ezetimibe or PCSK9 inhibitors, may be required to achieve target lipid levels (Grundy et al., 2018).
Antiplatelet Therapy
Antiplatelet therapy, usually with aspirin or clopidogrel, is often prescribed to prevent the formation of blood clots in individuals with a history of heart attack or stroke. Dual antiplatelet therapy (DAPT) may be recommended for certain patients, particularly those with a recent acute coronary syndrome or who have undergone stent placement (Capodanno et al., 2018).
Lifestyle Changes
In addition to pharmacological interventions, lifestyle changes play a pivotal role in managing cardiovascular risk. Smoking cessation, dietary modifications, regular physical activity, and weight management are all essential components of a comprehensive risk reduction strategy.
Special Considerations in Specific Populations
Elderly Patients
Older adults often present unique challenges in managing blood sugar levels and cardiovascular risk. They may have multiple comorbidities, polypharmacy, and an increased risk of hypoglycemia. In this population, a less stringent HbA1c target of 7.5-8.0% may be appropriate to balance the benefits of tight glycemic control with the risks of hypoglycemia and other adverse effects (American Diabetes Association, 2020).
Patients with Renal Impairment
Chronic kidney disease (CKD) is common in individuals with diabetes and cardiovascular disease. Renal impairment affects the metabolism and excretion of many medications, necessitating dose adjustments and careful monitoring. Some antihyperglycemic agents, such as metformin and certain SGLT2 inhibitors, have shown renal benefits and may be preferred in this population (Perkovic et al., 2019).
Future Directions and Research
Despite significant advancements in the management of blood sugar levels and cardiovascular risk, there remain areas for further research and improvement. Future studies should focus on:
1. Personalized Medicine: Developing individualized treatment plans based on genetic, phenotypic, and lifestyle factors to optimize blood sugar control and reduce cardiovascular risk.
2. Novel Therapeutics: Investigating new pharmacological agents and treatment modalities that target both glycemic control and cardiovascular risk reduction.
3. Long-Term Outcomes: Evaluating the long-term benefits and risks of intensive glycemic control in different populations, including elderly patients and those
with multiple comorbidities.
4. Patient Education and Engagement: Enhancing patient education and self-management strategies to empower individuals to take an active role in their care and improve adherence to treatment plans.
Conclusion
Maintaining optimal blood sugar levels is vital for preventing repeat strokes and heart attacks in individuals with a history of these conditions. Current guidelines suggest that targets should be individualized, with a general recommendation of keeping HbA1c levels below 7%, and potentially as low as 6.5% in certain high-risk patients. A combination of lifestyle modifications, pharmacological interventions, and continuous monitoring is essential to achieve these goals and reduce the risk of recurrent cardiovascular events. Comprehensive cardiovascular risk management, addressing hypertension, dyslipidemia, and other modifiable risk factors, is equally important in this population. Further research is needed to refine these targets and develop more effective strategies for blood sugar management in this vulnerable population.
References
– American Heart Association. (2020). Cardiovascular Disease and Diabetes. Retrieved from https://www.heart.org
– Capodanno, D., Angiolillo, D. J., & Bhatt, D. L. (2018). Dual antiplatelet therapy for secondary prevention of cardiovascular disease. Journal of the American College of Cardiology, 72(19), 2306-2325.
– Galleon
– Ideal Blood Sugar Levels for Preventing Repeat Strokes and Heart Attacks
StrictionD: Your Ultimate Guide to Natural Blood Sugar Control

One thought on “Ideal Blood Sugar Levels for Preventing Repeat Strokes and Heart Attacks”