Introduction to Inflammatory Bowel Disease (IBD)
Inflammatory bowel disease (IBD) is an umbrella term used to describe disorders that involve chronic inflammation of the digestive tract. The two main types of IBD are ulcerative colitis and Crohn’s disease. Both conditions involve an abnormal immune response that results in inflammation and damage to the gastrointestinal tract, but they affect different areas and have distinct characteristics.
Types of IBD: Ulcerative Colitis and Crohn’s Disease
Ulcerative Colitis (UC): Ulcerative colitis actively limits itself to the colon (large intestine) and the rectum. Inflammation occurs only in the innermost lining of the colon, causing ulcers or sores. Symptoms of UC include bloody diarrhea, abdominal cramps, and a frequent urge to have bowel movements. Severe cases may also present with fatigue, fever, and weight loss.
Crohn’s Disease: Unlike UC, Crohn’s disease can affect any part of the gastrointestinal tract, from the mouth to the anus. The inflammation in Crohn’s disease can penetrate deep into the layers of the affected bowel tissue. Common symptoms include diarrhea, abdominal pain, and weight loss. More severe cases can lead to fatigue, fever, and malnutrition.
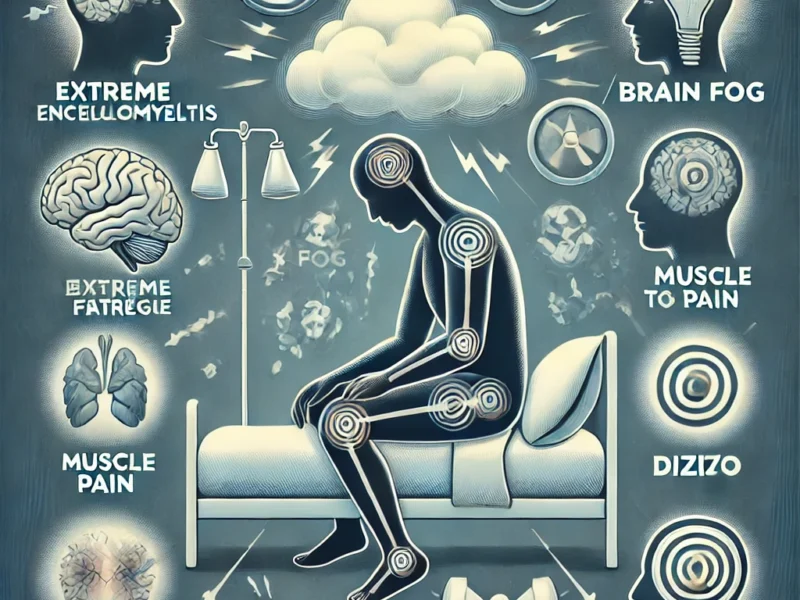
Symptoms and Complications
Symptoms: The symptoms of Inflammatory bowel disease (IBD) vary depending on the location and severity of inflammation but generally include persistent diarrhea, abdominal pain, rectal bleeding, weight loss, and fatigue. In some cases, individuals may also experience reduced appetite, fever, and growth delays in children.
Complications: IBD can lead to several complications. Both ulcerative colitis and Crohn’s disease increase the risk of colon cancer. Other potential complications include bowel obstructions, malnutrition, fistulas, and fissures. Additionally, IBD can cause inflammation in other parts of the body, such as the skin, eyes, and joints, and increase the risk of blood clots.
Causes and Risk Factors
The exact cause of IBD remains unknown, but researchers believe it actively results from a combination of genetic, environmental, and immune system factors. Genetics play a significant role, as IBD tends to run in families. Environmental factors, such as diet and stress, can also trigger or exacerbate the condition. The immune system’s abnormal response to bacteria in the gut is another critical factor.
Diagnosis of IBD
Diagnosing IBD involves a combination of medical history, physical examination, and diagnostic tests. Common diagnostic procedures include:
- Blood tests: To check for anemia and signs of inflammation.
- Stool tests: To detect blood or pathogens.
- Endoscopic procedures: Such as colonoscopy and flexible sigmoidoscopy, to visualize the colon and obtain tissue samples.
- Imaging tests: Including MRI and CT scans, to assess the extent of inflammation and detect complications like fistulas or abscesses.
Treatment Options
The primary goal of IBD treatment is to reduce inflammation, manage symptoms, and achieve and maintain remission. Treatment approaches include:
Medications:
- Anti-inflammatory drugs: Medications such as aminosalicylates and corticosteroids actively reduce inflammation.
- Immune system suppressors: Including azathioprine, methotrexate, and biologics, help to modulate the immune response.
- Antibiotics: For infections and specific complications of Crohn’s disease.
- Other medications: Like antidiarrheal agents, pain relievers, and nutritional supplements.
Surgery: Surgery may be necessary for patients who do not respond to medication or develop complications. Procedures can include resection of affected bowel segments, strictureplasty to widen narrowed sections, and colectomy to remove the colon in severe cases of ulcerative colitis.
Lifestyle and Dietary Considerations
Diet and lifestyle modifications play an essential role in managing IBD. While there is no specific diet for IBD, certain dietary changes can help manage symptoms. Healthcare providers actively advise patients to avoid trigger foods, eat smaller meals, stay hydrated, and keep a food diary to track which foods exacerbate their symptoms. Stress reduction techniques, regular exercise, and quitting smoking are also beneficial.
Gut Microbiota and IBD
Emerging research suggests that the gut microbiota, the community of microorganisms living in the intestines, plays a significant role in IBD. Research has actively associated dysbiosis, or an imbalance in the gut microbiota, with the development and progression of IBD. Studies are ongoing to explore how modifying the gut microbiota through diet, probiotics, and fecal microbiota transplantation could potentially benefit IBD patients.
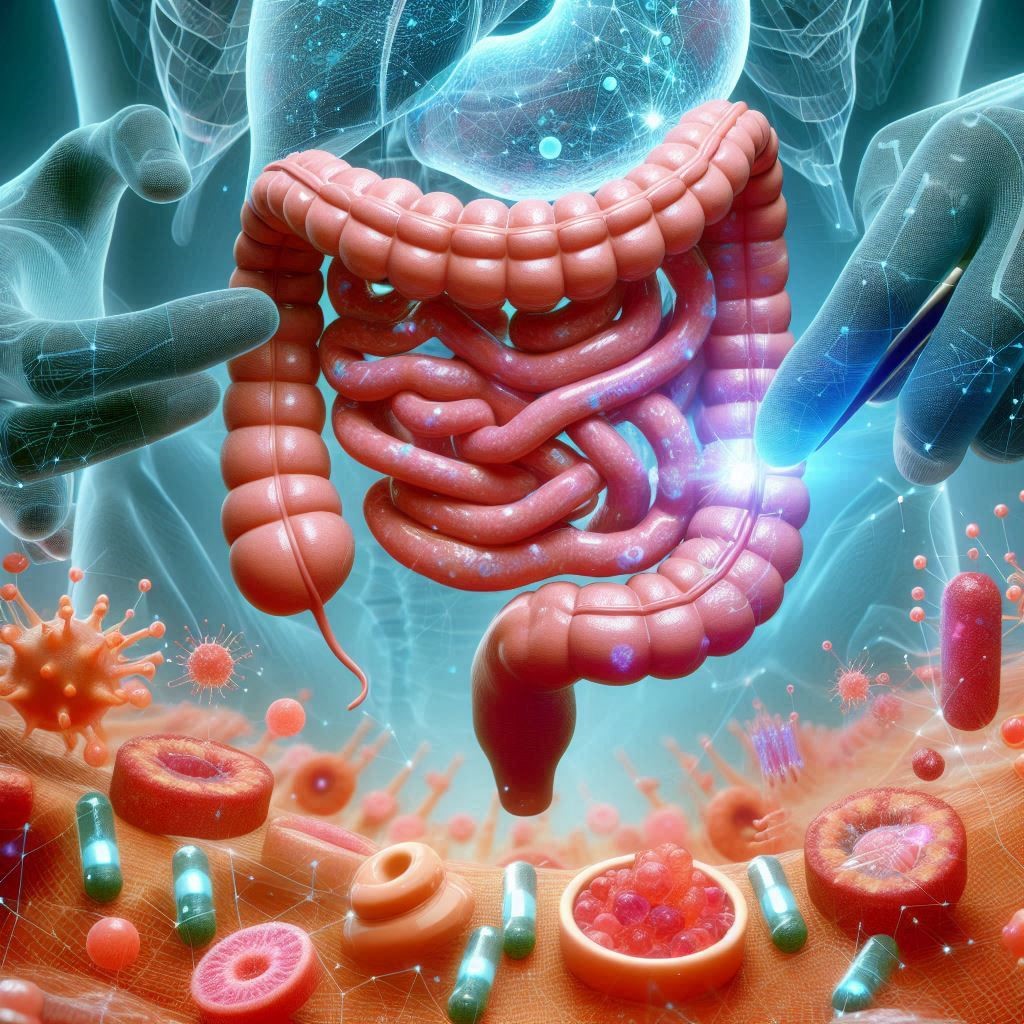
Microbotics in the Treatment of IBD
One of the innovative approaches to treating IBD involves the use of microbotics. Microbots, tiny robots often less than a millimeter in size, are being developed for targeted drug delivery and precise interventions within the gastrointestinal tract.
Targeted Drug Delivery: Microbots can be engineered to deliver medications directly to the inflamed areas of the gastrointestinal tract. This approach minimizes systemic side effects and maximizes the therapeutic effect at the site of inflammation. Researchers are exploring various types of microbots, including those that can be ingested and navigate through the digestive system to release drugs at specific locations.
Non-Invasive Procedures: Microbots can perform non-invasive procedures such as biopsies or removing obstructions without the need for major surgery. This can significantly reduce recovery times and the risk of complications compared to traditional surgical methods.
Monitoring and Diagnostics: Microbots equipped with sensors can provide real-time monitoring of the gastrointestinal environment. They can measure pH levels, detect inflammation markers, and even perform imaging, providing valuable data for diagnosing and managing IBD. These microbots can be controlled wirelessly, allowing for precise navigation and operation within the body.
Innovations and Future Directions
The management of IBD is continuously evolving with advancements in research and technology. Newer biologic therapies and small molecule drugs offer promising options for patients with moderate to severe IBD. Personalized medicine, where treatment is tailored to an individual’s genetic makeup and disease characteristics, is another area of active research. Additionally, ongoing studies aim to better understand the role of the gut microbiome and develop targeted therapies to restore a healthy balance of gut bacteria.
External Links for Further Reading
- Mayo Clinic: IBD
- Cleveland Clinic: IBD
- Johns Hopkins Medicine: IBD
Conclusion
Inflammatory bowel disease is a complex and chronic condition that requires a comprehensive approach to diagnosis, treatment, and management. By understanding the types, symptoms, and treatment options for IBD, patients and healthcare providers can work together to achieve the best possible outcomes. Ongoing research and advancements in medicine continue to provide hope for improved therapies and a better quality of life for those living with IBD.
Microbotics represents a cutting-edge avenue for the treatment and management of IBD. By offering precise, targeted interventions, microbots hold the potential to revolutionize the way IBD is treated, reducing side effects and improving patient outcomes. As research in this area progresses, the integration of microbotics in clinical practice may become a standard component of IBD management.