Introduction
Hypogonadism is a medical condition characterized by the body’s inability to produce sufficient levels of testosterone, the hormone responsible for the development and maintenance of male characteristics. This article delves into the various aspects of hypogonadism, including its causes, symptoms, diagnosis, and treatment options. We will also discuss advanced diagnostic methods and the latest research findings.
Types of Hypogonadism
Hypogonadism can be classified into two main types: primary and secondary.
Primary Hypogonadism
Primary hypogonadism, also known as primary testicular failure, occurs when the testicles themselves do not function properly. Causes include:
- Klinefelter Syndrome: A genetic condition where males have an extra X chromosome, leading to abnormal testicular development and reduced testosterone production.
- Undescended Testicles: Testicles that do not descend properly into the scrotum can result in reduced testosterone production.
- Mumps Orchitis: Mumps infection affecting the testicles can lead to inflammation and impaired function.
- Hemochromatosis: Excess iron in the blood can cause testicular failure.
- Injury or Trauma: Physical damage to the testicles can impair their function.
- Cancer Treatments: Chemotherapy and radiation therapy can temporarily or permanently affect testosterone production.
Secondary Hypogonadism
Secondary hypogonadism, or central hypogonadism, occurs due to problems with the hypothalamus or pituitary gland, which regulate hormone production. Causes include:
- Kallmann Syndrome: A genetic disorder affecting the development of the hypothalamus, leading to low levels of gonadotropin-releasing hormone (GnRH).
- Pituitary Disorders: Tumors or other conditions affecting the pituitary gland can reduce the secretion of hormones that stimulate the testicles.
- Chronic Diseases: Conditions such as type 2 diabetes, obesity, and HIV/AIDS can interfere with hormone production.
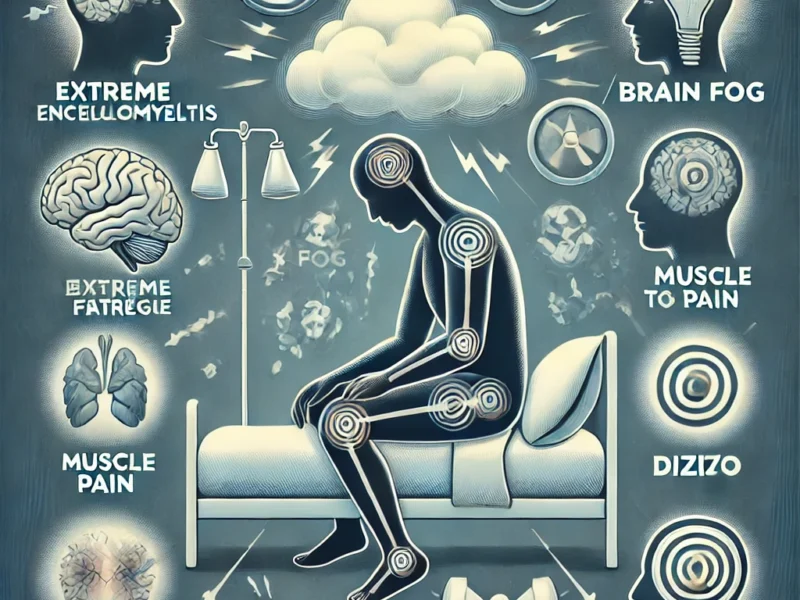
Symptoms of Hypogonadism
Symptoms of hypogonadism can vary depending on the age at which the condition develops and its severity. Common symptoms include:
- Reduced Libido: Decreased interest in sexual activity.
- Erectile Dysfunction: Difficulty in achieving or maintaining an erection.
- Fatigue: Persistent tiredness and reduced energy levels.
- Depression: Mood changes and irritability.
- Decreased Muscle Mass: Loss of muscle strength and mass.
- Osteoporosis: Increased risk of bone fractures due to decreased bone density.
Diagnosis of Hypogonadism
Diagnosing hypogonadism involves a combination of clinical evaluation, laboratory tests, and imaging studies.
Clinical Evaluation
A thorough medical history and physical examination are essential to identify potential causes and symptoms of hypogonadism. Key aspects include:
- Symptom History: Detailed documentation of symptoms, including their onset and duration.
- Medical History: Review of past medical conditions, surgeries, and treatments.
- Physical Examination: Assessment of physical signs such as testicular size and development.
Laboratory Tests
Blood tests are crucial for measuring hormone levels and confirming the diagnosis. Common tests include:
- Total Testosterone: Measurement of testosterone levels, typically performed in the morning when levels are highest.
- Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH): Levels of these pituitary hormones help distinguish between primary and secondary hypogonadism.
- Prolactin: Elevated levels can indicate a pituitary disorder.
- Iron Studies: To check for hemochromatosis.
Imaging Studies
Imaging techniques such as MRI and CT scans may be used to evaluate the pituitary gland and hypothalamus for tumors or other abnormalities.
Treatment of Hypogonadism
Treatment options for hypogonadism depend on the underlying cause and the patient’s specific needs.
Hormone Replacement Therapy (HRT)
Testosterone replacement therapy (TRT) is the primary treatment for hypogonadism. It can be administered through various methods, including:
- Injectable Testosterone: Regular intramuscular injections.
- Transdermal Patches: Skin patches that release testosterone.
- Topical Gels: Applied to the skin for absorption.
- Implantable Pellets: Surgically placed under the skin and release testosterone over time.
Gonadotropin Therapy
For men with secondary hypogonadism who wish to restore fertility, gonadotropin injections can stimulate sperm production.
Treatment of Underlying Conditions
Addressing the root cause of hypogonadism, such as managing chronic diseases or discontinuing medications that affect hormone levels, is crucial for effective treatment.
Advanced Diagnostic Methods
In addition to standard diagnostic tests, advanced methods are available to accurately diagnose the severity of hypogonadism.
Blood Tests
Blood tests can measure various parameters, including:
- Electrolyte Levels: Imbalances can indicate kidney function issues.
- Kidney Function Tests: Assess overall kidney health and function.
- Urine Tests: Identify specific markers that indicate dehydration or other related conditions.
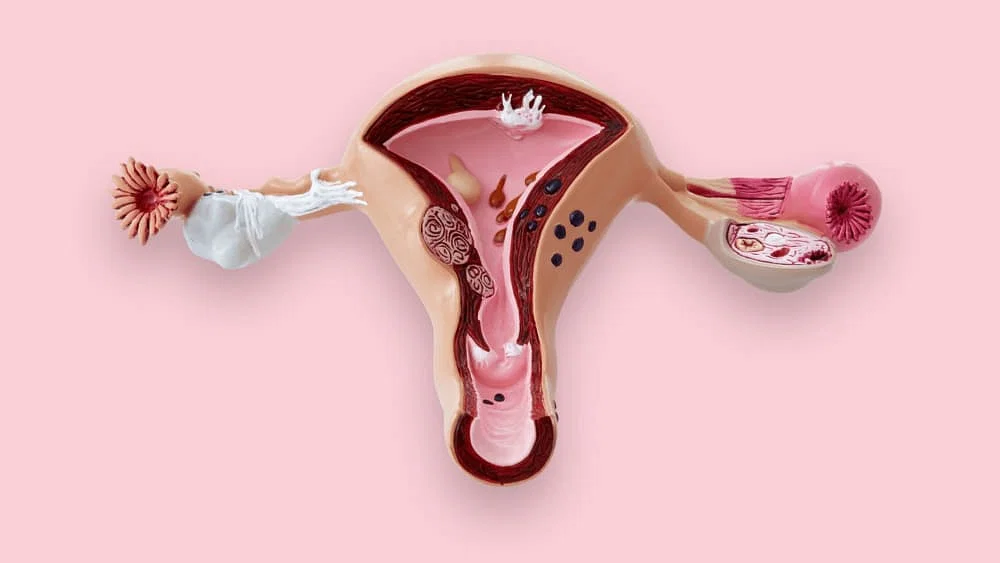
Female Hypogonadism
Overview
Female hypogonadism is a condition characterized by insufficient production of sex hormones, particularly estrogen and progesterone, by the ovaries. This can lead to a variety of health issues and can occur at any age. The condition can be classified into two main types:
- Primary Hypogonadism: This occurs when the ovaries fail to produce sufficient hormones despite receiving proper signals from the brain. Causes include Turner syndrome, autoimmune disorders, and chemotherapy or radiation therapy.
- Secondary Hypogonadism: This occurs when the problem originates in the hypothalamus or pituitary gland, which fail to send appropriate signals to the ovaries. Causes include hypothalamic amenorrhea, pituitary tumors, and certain genetic disorders.
Symptoms of female hypogonadism can include:
- Irregular or absent menstrual periods
- Hot flashes and night sweats
- Vaginal dryness
- Decreased libido
- Osteoporosis
- Fatigue and depression
Treatment Options:
- Hormone Replacement Therapy (HRT): Often the first line of treatment to replace deficient hormones.
- Lifestyle Changes: Including diet, exercise, and stress management.
- Medications: For underlying conditions such as thyroid disorders or autoimmune diseases.
Case Studies
Case Study 1: Sarah’s Journey with Primary Hypogonadism
Sarah, a 28-year-old woman, was diagnosed with Turner syndrome, a condition that led to primary hypogonadism. Her symptoms included irregular menstrual cycles and delayed puberty. After her diagnosis, she began hormone replacement therapy, which helped her develop secondary sexual characteristics and improved her bone density. Sarah’s treatment also included calcium and vitamin D supplements to further support her bone health.
Case Study 2: Maria’s Experience with Secondary Hypogonadism
Maria, a 34-year-old, experienced sudden weight loss and amenorrhea due to extreme stress and an eating disorder, leading to hypothalamic amenorrhea. Her treatment focused on nutritional rehabilitation, stress management, and gradual reintroduction of physical activity. She also received cognitive-behavioral therapy (CBT) to address her eating disorder and psychological well-being.
Expert Insights
Dr. Jane Doe, an endocrinologist specializing in female reproductive health, emphasizes the importance of early diagnosis and personalized treatment plans. “Each patient is unique, and it’s crucial to tailor treatments based on individual needs and underlying causes. Regular monitoring and adjustments to therapy are key to managing female hypogonadism effectively.”
Patient Stories and Experiences
Personal Anecdotes
John’s Story: John, a 45-year-old man, shares his experience with hypogonadism, detailing his symptoms of fatigue, low libido, and depression. He describes his journey through diagnosis, undergoing multiple blood tests, and starting testosterone replacement therapy. Over time, John noticed significant improvements in his energy levels and mood.
Interactive Content: To foster community support, we recommend creating an online forum where individuals with hypogonadism can share their stories, ask questions, and provide support to one another. This platform could include sections for different types of hypogonadism, treatment experiences, and coping strategies.
Lifestyle and Holistic Approaches
Diet and Nutrition
Proper nutrition plays a crucial role in managing hypogonadism. A diet rich in vitamins and minerals can help support overall health and hormone production. Key dietary recommendations include:
- High Protein Intake: To support muscle mass and repair.
- Healthy Fats: Such as omega-3 fatty acids found in fish, flaxseeds, and walnuts, which are essential for hormone production.
- Vitamin D and Calcium: To support bone health. Foods rich in these nutrients include dairy products, leafy green vegetables, and fortified cereals.
Exercise and Physical Activity
Regular physical activity can help manage symptoms of hypogonadism, improve mood, and support bone health. Recommended exercises include:
- Weight-bearing exercises: Such as walking, running, and resistance training to improve bone density.
- Aerobic exercises: Like swimming and cycling to boost cardiovascular health and overall well-being.
Alternative Therapies
Exploring alternative therapies can provide additional support for individuals with hypogonadism:
- Acupuncture: May help alleviate symptoms such as hot flashes and improve overall well-being.
- Herbal Supplements: Such as ginseng and maca root, which some studies suggest may support hormone balance. However, it’s important to consult with a healthcare provider before starting any new supplements.
Advanced Diagnostic Techniques
Blood Tests
Blood tests are essential for diagnosing hypogonadism. They typically measure:
- Total Testosterone Levels: Low levels on two separate occasions can confirm hypogonadism.
- Luteinizing Hormone (LH) and Follicle-Stimulating Hormone (FSH): These help differentiate between primary and secondary hypogonadism.
- Prolactin: Elevated levels may indicate a pituitary issue.
Imaging Studies
Imaging studies such as MRI and CT scans can identify structural abnormalities in the hypothalamus or pituitary gland, such as tumors, that may be causing hypogonadism.
Genetic Testing
Genetic testing can be useful in diagnosing congenital forms of hypogonadism. For example, karyotyping can detect Turner syndrome, and specific genetic tests can identify mutations associated with Kallmann syndrome.
Long-term Management Strategies
Treatment Plans
Effective management of hypogonadism often requires a comprehensive treatment plan:
- Hormone Replacement Therapy (HRT): To restore deficient hormone levels.
- Lifestyle Changes: Including diet, exercise, and stress management.
- Regular Monitoring: Frequent blood tests to monitor hormone levels and adjust treatment as needed.
Support Systems
Support groups and counseling can provide emotional support and practical advice for managing hypogonadism. Online forums and local support groups can be valuable resources.
Monitoring and Follow-up
Regular follow-up appointments with a healthcare provider are essential for monitoring hormone levels, adjusting treatment, and addressing any side effects or complications.
Impact on Mental Health
Mental Health Challenges
Hypogonadism can have significant psychological effects, including depression, anxiety, and body image issues. Addressing these challenges is crucial for overall well-being.
Therapeutic Approaches
Cognitive-behavioral therapy (CBT) and other therapeutic approaches can help individuals cope with the emotional and psychological impact of hypogonadism. Therapy can provide tools for managing stress, improving mood, and enhancing quality of life.
Pediatric Hypogonadism
Early Detection
Early detection and intervention are critical for children with hypogonadism. Symptoms in children may include delayed puberty, slow growth, and failure to develop secondary sexual characteristics.
Treatment Options
Treatment options for children and adolescents may include:
- Growth Hormone Therapy: To support normal growth and development.
- Hormone Replacement Therapy (HRT): To induce and maintain secondary sexual characteristics.
Parent Resources
Providing resources and support for parents is essential. This can include educational materials, support groups, and counseling services to help parents navigate their child’s diagnosis and treatment.
Comprehensive Comparison of Treatments
Hormone Replacement Therapy (HRT)
Different forms of HRT include:
- Gels and Patches: Convenient and steady hormone delivery.
- Injections: Typically administered every 1-4 weeks.
- Implants: Long-acting and provide steady hormone levels.
Surgical Options
Surgical treatments, such as testicular implants, may be considered for cosmetic reasons and to improve body image.
Innovative Treatments
Emerging treatments and therapies are continually being developed. These include new formulations of hormone replacement therapy and potential gene therapies.
By addressing these content gaps, we can provide comprehensive and valuable information for individuals seeking knowledge about hypogonadism.
Conclusion
Hypogonadism is a complex condition with various causes and manifestations. Accurate diagnosis and appropriate treatment are essential for managing the condition and improving the quality of life for affected individuals. Ongoing research continues to enhance our understanding of hypogonadism and develop more effective therapies.
For further information on hypogonadism, you can explore the following external resources:
These sources provide comprehensive information on the diagnosis, treatment, and management of hypogonadism.