Lymphoma: A Comprehensive Overview
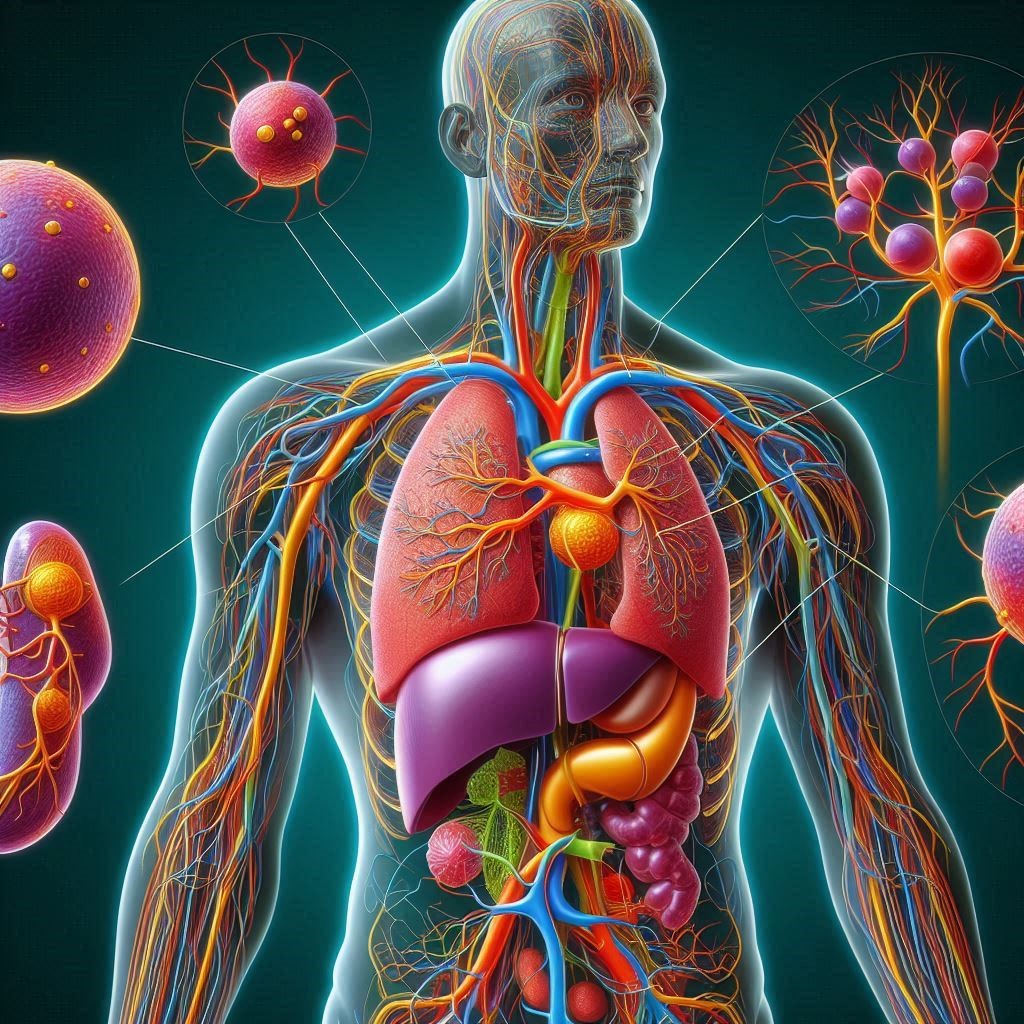
Lymphoma is a type of cancer that originates in the lymphatic system, specifically affecting the lymphocytes, a type of white blood cell integral to the immune system. Hodgkin lymphoma (HL) and non-Hodgkin lymphoma (NHL) are the two main types of lymphoma. They differ in characteristics, subtypes, and treatment approaches. Understanding these differences is crucial for proper diagnosis and care. This article delves into the epidemiology, pathophysiology, diagnosis, treatment, and ongoing research in the field of lymphoma.
Epidemiology and Risk Factors
Lymphoma represents a significant health burden worldwide, with varying incidence and prevalence across different regions. Hodgkin lymphoma accounts for approximately 10% of all lymphoma cases, while non-Hodgkin lymphoma is more common. Genetic predisposition, weak immune systems, certain infections, and exposure to pesticides/radiation all increase lymphoma risk.
Pathophysiology
Lymphomas originate from mutations in the DNA of lymphocytes, leading to uncontrolled cell growth and proliferation. In Hodgkin lymphoma, Reed-Sternberg cells, a type of abnormal B lymphocyte, are a hallmark of the disease. Non-Hodgkin lymphoma encompasses a diverse group of malignancies, each with unique genetic mutations and biological behavior. Common subtypes of NHL include diffuse large B-cell lymphoma (DLBCL), follicular lymphoma, and mantle cell lymphoma.
Lymphoma Diagnosis
Diagnosing lymphoma involves a combination of clinical evaluation, imaging studies, and histopathological examination. Key diagnostic tools include:
- Physical Examination: Checking for swollen lymph nodes, spleen, or liver.
- Imaging Studies: CT scans, PET scans, and MRI are used to identify the extent and spread of the disease.
- Biopsy: A lymph node biopsy is essential to confirm the diagnosis and subtype. Flow cytometry and immunohistochemistry are often used to characterize the lymphoma cells.
- Molecular Tests: Genetic testing and molecular profiling help identify specific mutations and guide treatment decisions.
Lymphoma Treatment
The treatment of lymphoma varies based on the type, stage, and individual patient factors. Standard treatment modalities include:
- Chemotherapy: Regimens such as CHOP (cyclophosphamide, doxorubicin, vincristine, and prednisone) are commonly used for NHL, while ABVD (doxorubicin, bleomycin, vinblastine, and dacarbazine) is standard for HL.
- Radiation Therapy: Often used in early-stage lymphoma or in combination with chemotherapy.
- Immunotherapy: Treatments like rituximab (a monoclonal antibody) and CAR T-cell therapy have revolutionized lymphoma care, particularly for refractory or relapsed cases.
- Stem Cell Transplant: High-dose chemotherapy followed by autologous or allogeneic stem cell transplant is considered for certain high-risk or relapsed lymphomas.
Advances in Immunotherapy
Immunotherapy has emerged as a promising approach for treating various types of lymphoma. CAR T-cell therapy, where a patient’s T cells are genetically modified to target cancer cells, has shown remarkable success. Four CAR T-cell therapies have been approved for different types of NHL, providing long-term remissions in a significant number of patients. Additionally, immune checkpoint inhibitors and novel bispecific antibodies are under investigation, offering new hope for patients with difficult-to-treat lymphomas.
Research and Future Directions
Ongoing research is focused on improving understanding of the disease’s genetic and molecular underpinnings, developing less toxic and more effective treatments, and exploring novel therapeutic approaches. Current studies are investigating the role of targeted therapies, such as BTK inhibitors and PI3K inhibitors, in managing specific subtypes of NHL. Additionally, research into the tumor microenvironment and its interaction with the immune system is providing insights that may lead to innovative treatments.
Tattoos May Increase The Chances of Lymphoma

Recent studies have examined potential connections between tattoos and an increased risk of lymphoma. Some researchers have identified that certain tattoo inks contain carcinogenic substances, such as polycyclic aromatic hydrocarbons (PAHs) and heavy metals, which may pose health risks. These substances have been shown to cause DNA damage and mutations in cell cultures, suggesting a theoretical risk for cancer development, including lymphoma.
A study published in the Archives of Toxicology highlighted that certain tattoo inks could lead to chronic inflammation and immune system activation, which might contribute to the development of lymphoproliferative disorders in genetically predisposed individuals. The study emphasized that while the overall risk is low, the potential for long-term exposure to harmful compounds in tattoo inks warrants further investigation.
Another investigation reported in Cancer Epidemiology, Biomarkers & Prevention found no significant increase in lymphoma incidence among individuals with tattoos compared to the general population. However, it noted isolated cases where lymphoma developed in tattooed skin areas, suggesting that localized immune responses to tattoo pigments might play a role in these rare instances.
While definitive evidence is lacking, these studies underscore the need for further research to fully understand the potential health implications of tattoo inks and their role in lymphoma risk. For more detailed information, refer to resources such as the National Cancer Institute and the Leukemia Society.
Summary
Lymphoma is a complex and heterogeneous group of cancers requiring a multifaceted approach to diagnosis and treatment. Advances in molecular biology and immunotherapy have significantly improved outcomes for many patients. Continued research and clinical trials are essential to further enhance our understanding and management of this disease. For more detailed information, refer to comprehensive resources such as the National Cancer Institute and the Leukemia Society.
Lymphoma in the Context of COVID-19
The COVID-19 pandemic has significantly impacted patients with lymphoma, presenting unique challenges in diagnosis, treatment, and overall care management. Here, we analyze these challenges and explore the adaptations made to mitigate their effects.
Diagnosis and Treatment Delays
During the pandemic, healthcare systems worldwide faced unprecedented strain, leading to delays in diagnostic procedures and treatment for many cancers, including lymphoma. Patients experienced postponed appointments and procedures due to resource reallocation and efforts to reduce COVID-19 transmission in healthcare settings. These delays can lead to disease progression, adversely affecting patient outcomes.
Risk of Severe COVID-19 Complications
Lymphoma patients, especially those undergoing treatment, are at increased risk of severe COVID-19 complications due to their compromised immune systems. Chemotherapy and other treatments can weaken immune defenses, making it harder to fight off infections. Studies have shown higher morbidity and mortality rates among lymphoma patients who contract COVID-19 compared to the general population.
Vaccination Recommendations
Vaccination against COVID-19 is strongly recommended for lymphoma patients. Research indicates that while these patients might have a reduced immune response to vaccines, vaccination still offers significant protection against severe disease. Booster doses are often recommended to enhance immunity. The timing of vaccination is crucial and should be coordinated with lymphoma treatment schedules to optimize efficacy and minimize potential interference with cancer therapy.
Telemedicine Advancements
The pandemic accelerated the adoption of telemedicine, providing a valuable tool for lymphoma patient care. Virtual consultations have become a common practice, allowing patients to maintain regular contact with their healthcare providers while minimizing exposure to COVID-19. Telemedicine has proven effective for routine follow-ups, medication management, and addressing patient concerns without the need for physical visits.
Strategies for Managing Lymphoma Care
Healthcare providers have implemented several strategies to manage lymphoma care during the pandemic effectively:
- Prioritization of Treatments: Critical treatments are prioritized, with adjustments made to less urgent procedures to reduce patient exposure to healthcare settings.
- Enhanced Safety Protocols: Strict infection control measures are in place in clinics and hospitals to protect immunocompromised patients.
- Patient Education: Patients are educated about the importance of hygiene, social distancing, and vaccination to prevent COVID-19 infection.
- Flexible Treatment Plans: Treatment regimens are adjusted as needed, including the use of oral therapies that can be taken at home to reduce hospital visits.
Summary
The COVID-19 pandemic has posed significant challenges for lymphoma patients, but the rapid adoption of telemedicine, strategic adjustments in treatment protocols, and vaccination efforts have helped mitigate these impacts. Continuous adaptation and patient education remain critical to managing effectively during ongoing and future health crises. For more detailed information, refer to resources such as the National Cancer Institute and the Leukemia & Lymphoma Society.
Recommended External Links
- National Cancer Institute – : Lymphoma Overview
- Leukemia & Lymphoma Society LLS
- Nature Outlook : Nature Outlook Lymphoma
These links provide comprehensive information and are valuable resources for anyone seeking to understand better.