
Introduction to Nociceptors
Nociceptors are specialized sensory receptors responsible for detecting and transmitting noxious stimuli, which are potentially harmful to tissues, thereby initiating the sensation of pain. These receptors play a crucial role in the body’s defense mechanism by alerting the central nervous system (CNS) to potential damage, allowing for protective responses. This article delves into the physiology, types, mechanisms, and clinical relevance of nociceptors, drawing on the latest scientific research and understanding.
Types of Nociceptors
Nociceptors can be broadly categorized into four types based on the nature of the stimuli they detect:
- Thermal Nociceptors: Respond to extreme temperatures.
- Mechanical Nociceptors: Triggered by physical damage such as cuts or pressure.
- Chemical Nociceptors: Activated by chemical stimuli from inflammation or external irritants.
- Polymodal Nociceptors: Respond to a combination of thermal, mechanical, and chemical stimuli.
Thermal Nociceptors
Thermal nociceptors respond to extreme heat (>45°C) or cold (<15°C). These receptors are found in both the skin and deeper tissues, where they detect potentially harmful temperature changes and signal this information to the CNS. Thermal nociception involves TRPV1 channels, which are activated by high temperatures and certain chemical agents like capsaicin .
Mechanical Nociceptors
Mechanical nociceptors are activated by physical forces such as pressure, pinch, or stretch that may cause tissue damage. They are typically involved in detecting sharp pain from cuts or blunt force. These nociceptors use mechanosensitive ion channels such as Piezo1 and Piezo2 to transduce mechanical stimuli into electrical signals .
Chemical Nociceptors
Chemical nociceptors are sensitive to various chemical substances that can cause tissue damage or inflammation. These include endogenous substances released during inflammation (e.g., bradykinin, prostaglandins) and exogenous irritants (e.g., capsaicin). Chemical nociceptors often utilize TRPA1 channels and GPCRs to detect these harmful chemicals .
Polymodal Nociceptors
Polymodal nociceptors are capable of responding to multiple types of noxious stimuli, including thermal, mechanical, and chemical. They are primarily found in the skin, viscera, and joints and play a significant role in the perception of complex pain. TRPV1 channels are a common feature of polymodal nociceptors, allowing them to detect a wide range of harmful stimuli.
Physiology of Nociception
The process of nociception involves four key steps: transduction, transmission, modulation, and perception.
Transduction Of Nociceptors
Transduction is the process by which nociceptors convert noxious stimuli into electrical signals. This occurs when noxious stimuli activate ion channels on the nociceptor membrane, leading to the generation of action potentials. Key channels involved in this process include TRP channels and voltage-gated sodium channels.
Transmission Of Nociceptors
Once an action potential is generated, it is transmitted along the axons of nociceptors to the spinal cord. Nociceptors primarily utilize Aδ fibers (thinly myelinated, fast-conducting) and C fibers (unmyelinated, slow-conducting) to transmit signals. Aδ fibers are associated with sharp, acute pain, while C fibers transmit dull, chronic pain.
Modulation Of Nociceptors
Modulation involves the alteration of pain signals within the spinal cord before they are relayed to higher brain centers. This can occur through various mechanisms, including the release of neurotransmitters and neuromodulators that enhance or inhibit pain signals. Key modulators include endogenous opioids, gamma-aminobutyric acid (GABA), and serotonin.
Perception Of Nociceptors
Perception is the final step, where pain signals are interpreted by the brain, resulting in the conscious experience of pain. This involves complex neural networks, including the thalamus, somatosensory cortex, insula, and anterior cingulate cortex. The integration of these signals allows for the discrimination of pain intensity, quality, and location.
Molecular Mechanisms in Nociceptors
Nociceptors express a variety of ion channels and receptors that detect noxious stimuli and initiate pain signaling. Key molecules include transient receptor potential (TRP) channels, voltage-gated sodium channels, and G-protein coupled receptors (GPCRs).
TRP Channels
TRP channels are a family of ion channels that detect thermal, mechanical, and chemical stimuli. Notable members include TRPV1, which responds to heat and capsaicin, and TRPA1, which is activated by cold and irritants. TRPV1 channels are also sensitive to protons and certain lipid metabolites, making them integral to the detection of a wide range of noxious stimuli .
Voltage-Gated Sodium Channels
Voltage-gated sodium channels, particularly Nav1.7, Nav1.8, and Nav1.9, play crucial roles in the initiation and propagation of action potentials in nociceptors. Mutations in these channels are associated with pain disorders such as inherited erythromelalgia and congenital insensitivity to pain. Nav1.7, in particular, is critical for pain signaling, and its inhibition has been shown to provide significant pain relief in animal models .
GPCRs
GPCRs, such as bradykinin receptors and prostaglandin receptors, mediate the effects of inflammatory mediators on nociceptors, sensitizing them and enhancing pain signals. GPCR activation leads to downstream signaling cascades that modulate ion channel activity and nociceptor excitability.
Clinical Relevance of Nociceptors
Nociceptors are central to various pain conditions, including acute pain, chronic pain, neuropathic pain, and inflammatory pain. Understanding their role is crucial for developing effective pain management strategies.
Acute Pain
Acute pain is a protective response to immediate tissue damage, often mediated by thermal and mechanical nociceptors. It typically resolves once the underlying cause is addressed. For example, the sharp pain experienced after a cut or burn is a direct result of nociceptor activation .
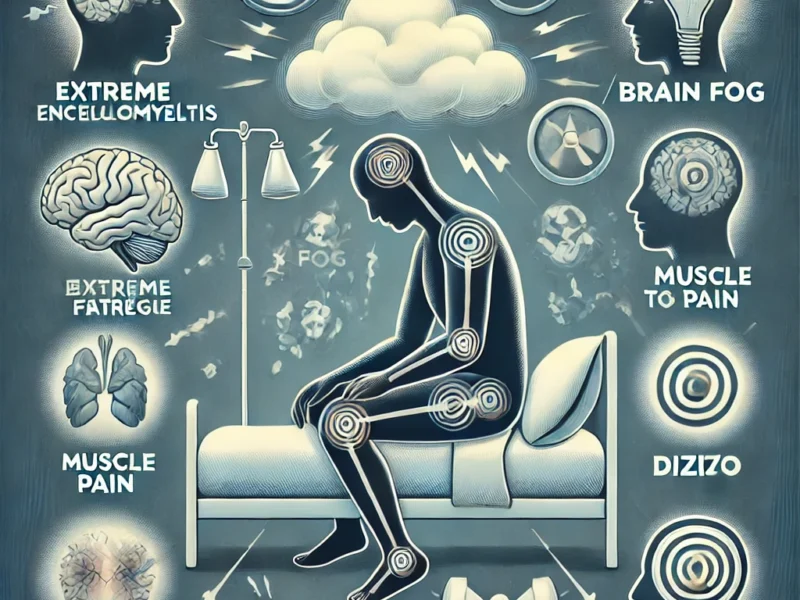
Chronic Pain
Chronic pain persists beyond the normal healing period and involves complex changes in nociceptor function and central pain processing. Conditions such as osteoarthritis, fibromyalgia, and chronic low back pain are examples. Chronic pain often results from persistent nociceptor sensitization and changes in central neural circuits that amplify pain signals .
Neuropathic Pain
Neuropathic pain arises from damage to the nervous system, leading to abnormal nociceptor activity and pain signaling. This can result from conditions like diabetes, shingles, and spinal cord injuries. Neuropathic pain is often characterized by burning, shooting, or electric shock-like sensations, and it can be particularly challenging to treat .
Inflammatory Pain
Inflammatory pain is associated with tissue inflammation, where nociceptors are sensitized by inflammatory mediators. Rheumatoid arthritis and inflammatory bowel disease are examples. Inflammatory pain involves the release of cytokines and growth factors that enhance nociceptor excitability and prolong pain signals .
Recent Advances in Nociceptor Research
Recent research has focused on understanding the molecular and cellular mechanisms of nociceptors to identify new therapeutic targets for pain management.
Neuroimmune Interactions
Emerging studies highlight the role of neuroimmune interactions in nociceptor sensitization and pain. For example, immune cells such as macrophages release inflammatory mediators that sensitize nociceptors, contributing to chronic pain conditions. Neuroimmune interactions are a promising area for developing new pain treatments that target both the nervous and immune systems .
PD-L1/PD-1 Pathway
The PD-L1/PD-1 pathway, known for its role in immune regulation, has been implicated in pain modulation. Studies suggest that targeting this pathway could offer new pain relief strategies, particularly in conditions involving neuroinflammation. For instance, blocking PD-L1 can modulate immune cell activity and reduce pain in animal models .
Nociceptor Plasticity
Nociceptor plasticity, the ability of nociceptors to change their function in response to injury or inflammation, is a key area of research. Understanding these changes could lead to novel interventions for preventing the transition from acute to chronic pain. Plasticity involves alterations in ion channel expression, receptor sensitivity, and synaptic connectivity, all of which contribute to persistent pain states .
Genetic and Epigenetic Factors
Genetic and epigenetic factors play significant roles in nociceptor function and pain susceptibility. Variations in genes encoding ion channels, receptors, and signaling molecules can influence individual pain sensitivity and response to pain treatments. Epigenetic modifications, such as DNA methylation and histone acetylation, can also regulate gene expression in nociceptors, affecting pain signaling pathways .
Future Directions in Nociceptor Research
The study of nociceptors, the sensory neurons responsible for detecting pain, is critical for developing advanced pain management strategies. The future directions in nociceptor research are focused on understanding the intricate mechanisms of pain perception, identifying novel therapeutic targets, and developing personalized pain treatments. This section highlights the most promising areas of research and their potential impact on pain therapy.
Neuroimmune Interactions in Pain
Role of Immune Cells in Nociceptor Sensitization
Recent studies have revealed significant interactions between the nervous and immune systems in the context of pain. Immune cells such as macrophages, mast cells, and T cells release cytokines and chemokines that can sensitize nociceptors and contribute to chronic pain. Understanding these interactions can lead to novel pain therapies that target both the nervous and immune systems to reduce nociceptor sensitization and alleviate pain.
Modulating Neuroinflammation
Neuroinflammation, characterized by the activation of glial cells and the release of pro-inflammatory mediators, plays a crucial role in the maintenance of chronic pain. Research is focusing on ways to modulate neuroinflammatory pathways to prevent or reverse pain sensitization. For instance, inhibiting the activation of microglia and astrocytes in the spinal cord and brain could provide new avenues for treating chronic pain conditions.
Genetic and Epigenetic Contributions to Pain
Genetic Variability in Pain Perception
Individual differences in pain sensitivity and chronic pain susceptibility are influenced by genetic factors. Research in this area aims to identify genetic variants associated with pain disorders, such as mutations in voltage-gated sodium channels (e.g., Nav1.7) or TRP channels (e.g., TRPV1). Understanding these genetic contributions can help in developing personalized pain management strategies that take into account a patient’s genetic makeup.
Epigenetic Modifications and Pain
Epigenetic changes, such as DNA methylation and histone acetylation, can regulate gene expression in nociceptors and influence pain pathways. Investigating these modifications can provide insights into the mechanisms of pain chronification and identify potential targets for epigenetic therapies. For example, targeting histone deacetylases (HDACs) has shown promise in preclinical studies for reducing chronic pain.
Advances in Pain Modulation Techniques
Neuromodulation Therapies
Neuromodulation involves the use of electrical or magnetic stimulation to alter neural activity and reduce pain. Techniques such as spinal cord stimulation (SCS), transcutaneous electrical nerve stimulation (TENS), and deep brain stimulation (DBS) are being refined to improve their efficacy and reduce side effects. Research is also exploring the use of closed-loop systems that adjust stimulation parameters in real-time based on feedback from the patient’s nervous system.
Optogenetics in Pain Research
Optogenetics, which involves the use of light to control genetically modified neurons, offers precise control over nociceptor activity and pain pathways. This technique allows researchers to selectively activate or inhibit specific populations of nociceptors, providing valuable insights into pain mechanisms and potential therapeutic targets. Optogenetics holds promise for developing highly targeted pain treatments with minimal off-target effects.
Novel Therapeutic Targets
Ion Channels and Receptors
Identifying new ion channels and receptors involved in nociceptor activation and sensitization is a key focus of pain research. For instance, the Nav1.7 sodium channel has emerged as a critical target for pain therapy, with several Nav1.7 inhibitors currently under investigation. Additionally, targeting TRP channels, such as TRPV1 and TRPA1, could provide new pain relief options for patients with chronic pain.
GPCRs and Pain Modulation
G-protein coupled receptors (GPCRs) play a vital role in mediating the effects of inflammatory mediators on nociceptors. Research is exploring the therapeutic potential of modulating GPCR activity to reduce pain. For example, bradykinin receptor antagonists and prostaglandin receptor inhibitors have shown promise in preclinical studies for treating inflammatory pain.
Personalized Pain Management
Pharmacogenomics in Pain Therapy
Pharmacogenomics, the study of how genetic variations affect drug response, is paving the way for personalized pain management. By identifying genetic markers that predict a patient’s response to specific pain medications, clinicians can tailor treatments to improve efficacy and reduce adverse effects. For example, genetic testing can help determine the optimal dose of opioids or the suitability of certain NSAIDs for individual patients.
Tailoring Treatments Based on Nociceptor Profiles
Advances in molecular biology and genomics allow for the characterization of individual nociceptor profiles. Understanding the specific ion channels, receptors, and signaling pathways involved in a patient’s pain can guide the selection of targeted therapies. Personalized pain management strategies can significantly enhance treatment outcomes and reduce the burden of chronic pain.
Integration of Neuroimaging and Genomics
Combining Neuroimaging and Genetic Data
Integrating neuroimaging techniques with genetic and epigenetic data can provide comprehensive insights into the central and peripheral mechanisms of pain. Neuroimaging methods such as functional MRI (fMRI) and positron emission tomography (PET) can visualize brain activity and connectivity patterns associated with pain perception. Combining these data with genomic studies can help identify biomarkers and therapeutic targets for pain.
Advances in Imaging Technologies
Recent advances in imaging technologies, such as high-resolution MRI and optogenetic imaging, are enhancing our ability to study nociceptor function and pain pathways in vivo. These technologies allow for the real-time observation of neural activity and the effects of pain treatments at a cellular and molecular level. Continued development of these imaging techniques will further our understanding of pain mechanisms and support the development of novel therapies.
Exploring New Models and Approaches
Animal Models of Pain
Animal models remain essential for studying nociceptor function and pain mechanisms. Researchers are developing more sophisticated models that better replicate human pain conditions, such as transgenic mice with humanized pain pathways. These models can provide valuable insights into the molecular and cellular mechanisms of pain and support the preclinical testing of new pain therapies.
Human-Based Models
In addition to animal models, human-based models such as induced pluripotent stem cells (iPSCs) and organ-on-a-chip technologies are being used to study nociceptors and pain pathways. iPSCs can be differentiated into sensory neurons, allowing for the investigation of human nociceptor function and the effects of genetic variations on pain. Organ-on-a-chip technologies provide a platform for studying pain in a more physiologically relevant context, bridging the gap between in vitro and in vivo research.
Conclusion
The future of nociceptor research holds great promise for advancing our understanding of pain mechanisms and developing innovative pain therapies. By exploring neuroimmune interactions, genetic and epigenetic contributions, novel therapeutic targets, and personalized pain management strategies, researchers aim to improve pain relief and enhance the quality of life for individuals suffering from chronic pain. Integrating cutting-edge technologies such as optogenetics, neuromodulation, and advanced imaging techniques will further our knowledge of nociceptor function and support the development of targeted, effective pain treatments. As we continue to unravel the complexities of nociception and pain, the prospects for better pain management and relief are brighter than ever.
Recommended External Links
- National Institute of Neurological Disorders and Stroke – Pain
- Healthline – Pain: Types, Symptoms, and Treatments
- Mayo Clinic – Chronic Pain: Symptoms and Causes
These resources provide additional information on pain types, symptoms, and management strategies, complementing the insights discussed in this review.
Nociceptor Function and Pain Mechanisms: Detailed Insights
Ion Channels and Receptors in Nociceptors
Nociceptors are equipped with a variety of ion channels and receptors that detect noxious stimuli and initiate pain signaling. Understanding the function of these molecular components is crucial for developing targeted pain therapies.
Transient Receptor Potential (TRP) Channels
TRP channels are a diverse family of ion channels that respond to thermal, mechanical, and chemical stimuli. TRPV1, TRPA1, and TRPM8 are notable members involved in nociception:
- TRPV1: Activated by heat (>43°C), capsaicin, and acidic pH, TRPV1 plays a key role in thermal nociception and inflammatory pain. Blocking TRPV1 has been shown to reduce pain in various animal models.
- TRPA1: Responds to cold temperatures, mechanical stress, and irritant chemicals such as mustard oil and acrolein. TRPA1 is involved in both acute and chronic pain conditions.
- TRPM8: Activated by cold temperatures and cooling agents like menthol, TRPM8 mediates cold-induced pain and contributes to the sensation of cooling relief in certain pain states.
Voltage-Gated Sodium Channels
Voltage-gated sodium channels, particularly Nav1.7, Nav1.8, and Nav1.9, are essential for the initiation and propagation of action potentials in nociceptors:
- Nav1.7: Highly expressed in nociceptors, Nav1.7 is critical for pain signal transmission. Genetic mutations in Nav1.7 can lead to either congenital insensitivity to pain or increased pain sensitivity, highlighting its importance in pain modulation.
- Nav1.8 and Nav1.9: These channels are primarily expressed in peripheral sensory neurons and contribute to the transmission of pain signals, especially under inflammatory and neuropathic conditions. Blocking these channels has shown analgesic effects in preclinical studies.
G-Protein Coupled Receptors (GPCRs)
GPCRs mediate the effects of various inflammatory mediators and modulate nociceptor activity:
- Bradykinin Receptors (B1 and B2): Bradykinin is a potent inflammatory mediator that sensitizes nociceptors and enhances pain. Blocking bradykinin receptors can reduce inflammatory pain.
- Prostaglandin Receptors (EP1-EP4): Prostaglandins are produced during inflammation and sensitize nociceptors via EP receptors. Nonsteroidal anti-inflammatory drugs (NSAIDs) reduce pain by inhibiting prostaglandin synthesis.
Central Processing of Pain
Nociceptive signals are processed in the spinal cord and transmitted to higher brain centers, where they are perceived as pain. Key regions involved in pain perception include:
- Spinal Cord Dorsal Horn: The first site of synaptic transmission for nociceptive signals. Here, primary afferent neurons synapse with second-order neurons, which then project to the brain.
- Thalamus: Acts as a relay station, transmitting nociceptive information from the spinal cord to the cortex.
- Somatosensory Cortex: Responsible for the localization and intensity of pain.
- Insula and Anterior Cingulate Cortex: Involved in the emotional and cognitive aspects of pain perception.
Neuroplasticity and Pain Chronicity
Neuroplasticity, the ability of neural circuits to change in response to experience, plays a significant role in the transition from acute to chronic pain. Changes in synaptic strength, receptor expression, and neural connectivity can lead to persistent pain states:
- Central Sensitization: Enhanced excitability of neurons in the spinal cord and brain due to repeated nociceptive input. Central sensitization contributes to chronic pain conditions by amplifying pain signals.
- Peripheral Sensitization: Increased sensitivity of nociceptors in response to injury or inflammation. Peripheral sensitization lowers the threshold for nociceptor activation, leading to heightened pain sensitivity.
Pain Management Strategies
Effective pain management requires a comprehensive understanding of nociceptor function and pain mechanisms. Current strategies include pharmacological, non-pharmacological, and interventional approaches:
Pharmacological Treatments
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Inhibit cyclooxygenase enzymes, reducing prostaglandin synthesis and inflammation.
- Opioids: Activate opioid receptors, providing potent analgesia but with a risk of dependence and side effects.
- Antidepressants and Anticonvulsants: Modulate neurotransmitter levels and neuronal excitability, effective for neuropathic pain.
- Topical Agents: Such as lidocaine and capsaicin, provide localized pain relief with minimal systemic effects.
Non-Pharmacological Treatments
- Physical Therapy: Improves mobility, strength, and pain management through exercises and manual techniques.
- Cognitive Behavioral Therapy (CBT): Addresses the psychological aspects of chronic pain, helping patients develop coping strategies.
- Acupuncture: Stimulates specific points on the body to modulate pain signals and promote healing.
Interventional Treatments
- Nerve Blocks: Involve the injection of anesthetics or steroids near nerves to interrupt pain signals.
- Spinal Cord Stimulation: Delivers electrical impulses to the spinal cord to reduce pain perception.
- Radiofrequency Ablation: Uses heat to destroy nerve fibers responsible for transmitting pain signals.
Conclusion
Nociceptors are integral to the body’s pain detection and response system, playing a critical role in both protective and pathological pain states. Understanding their function and mechanisms is essential for advancing pain management strategies and improving quality of life for individuals suffering from pain. Ongoing research into nociceptor biology, neuroimmune interactions, and neuroplasticity holds promise for developing novel and effective pain therapies.
Recommended External Links
- Healthline – Pain: Types, Symptoms, and Treatments
- Mayo Clinic – Chronic Pain: Symptoms and Causes
- National Institute of Neurological Disorders and Stroke – Pain
These resources provide additional information on pain types, symptoms, and management strategies, complementing the insights discussed in this review.
Recommended Internal Links
- Unlock Your Focus: Herberall – The Brainpower Booster
- Huntington’s Disease: From Genes to Therapies
- Memotenz Review: A Deep Dive into This Popular Nootropic Supplement
- Brain Exercise to Improve Cognition and Mental Health
- SuperBeets Memory and Focus Review: Hype or Help?
- Neuriva Plus for a More Focused, More Productive You
- Brain Hack or Brain Snack? Our No-Nonsense Review of Onnit Alpha Brain
- New Research Shows ‘Profound’ Link Between Dietary Choices and Brain Health

One thought on “Nociceptors: A Comprehensive Scholarly Review”