- Introduction to Epidural Administration
- History of Epidural Administration
- Mechanism of Action
- Indications for Epidural Administration
- Procedure for Epidural Administration
- Types of Epidural Injections
- Benefits of Epidural Administration
- Risks and Complications
- Managing Complications
- Post-Procedure Care
- Advances in Epidural Administration
- Clinical Studies and Research
- Future Directions and Innovations
- Conclusion
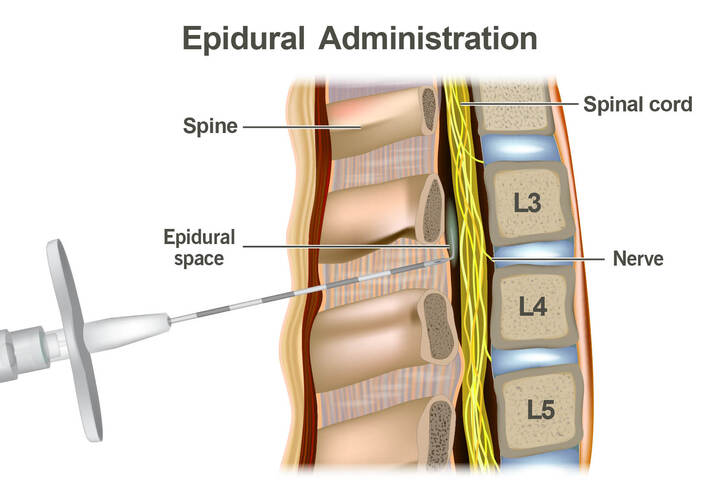
Introduction to Epidural Administration
Epidural administration is a prevalent and highly effective method of pain relief, extensively used in labor, surgical procedures, and chronic pain management. It involves the injection of anesthetic medication into the epidural space surrounding the spinal cord, blocking nerve impulses and thereby reducing pain sensation in specific areas of the body.
History of Epidural Administration
The history of epidural anesthesia dates back to the late 19th and early 20th centuries. In 1885, American neurologist James Leonard Corning performed the first documented epidural anesthesia, although inadvertently, while experimenting with cocaine. Corning’s work laid the foundation for further developments in regional anesthesia. The term “epidural” derives from the Greek word “epi,” meaning “upon,” and “dural,” referring to the dura mater, the tough outer membrane surrounding the spinal cord.
In 1901, French surgeon Jean-Anthanase Sicard and Italian surgeon Fernand Cathelin independently described the technique of injecting medication into the epidural space. However, it was not until the 1930s that the technique began to gain wider acceptance in medical practice. Significant advancements in the 1940s and 1950s included the introduction of continuous epidural anesthesia, where a catheter is placed in the epidural space to allow for prolonged drug administration. This development revolutionized pain management during labor and surgical procedures.
Mechanism of Action
Epidural medications typically consist of local anesthetics combined with opioids or narcotics. These drugs act on the nerve roots in the epidural space to block electrical impulses that transmit pain to the brain. The medication spreads both circumferentially and longitudinally, affecting several dermatomes depending on the injection site. Some of the medication may diffuse into the cerebrospinal fluid (CSF) and is eventually removed through vascular absorption.
Local Anesthetics: Commonly used local anesthetics include lidocaine, bupivacaine, and ropivacaine. These agents work by blocking sodium channels on nerve cells, preventing the initiation and transmission of nerve impulses. The onset of action typically occurs within 10 to 20 minutes, and the duration of anesthesia can last from a few hours to several days, depending on the type and amount of anesthetic used.
Opioids: Adding opioids like fentanyl or morphine to the epidural solution enhances pain relief by acting on opioid receptors in the spinal cord. This combination allows for lower doses of local anesthetics, reducing the risk of side effects associated with high doses of these drugs.
Indications for Epidural Administration
Epidural administration is used in various clinical scenarios, including:
- Labor and Delivery: Epidural anesthesia is commonly used during childbirth to provide pain relief while allowing the mother to remain awake and alert. It can be adjusted to provide varying levels of anesthesia, depending on the stage of labor and the mother’s comfort level.
- Major Surgeries: Epidurals are used in surgeries involving the lower abdomen, pelvis, and lower limbs, such as hip and knee replacements, abdominal surgeries, and cesarean sections. This technique provides effective pain control during and after the procedure.
- Chronic Pain Management: Epidural steroid injections are used to manage chronic pain conditions like sciatica, spinal stenosis, and herniated discs. These injections reduce inflammation and pain by delivering steroids directly to the affected area.
- Palliative Care: Epidural administration is also used in palliative care settings to manage intractable pain in patients with terminal illnesses, improving their quality of life.
Procedure for Epidural Administration
The procedure for administering an epidural involves several steps:
- Preparation: The patient is positioned to facilitate easy access to the lower back, usually sitting up or lying on their side. The area is cleaned and sterilized to prevent infection.
- Local Anesthesia: An area on the back is injected with local anesthetic to numb the skin and deeper tissues, reducing discomfort during the insertion of the epidural needle.
- Insertion: A needle is inserted into the epidural space, guided by the loss of resistance technique or imaging such as fluoroscopy. This involves passing the needle through various tissues and ligaments until it reaches the epidural space, identified by a sudden loss of resistance felt by the practitioner.
- Catheter Placement: A thin catheter is threaded through the needle into the epidural space, allowing continuous medication administration. The catheter is typically inserted 4 to 6 centimeters into the epidural space and secured in place.
- Monitoring: The patient is monitored for any adverse reactions, and the catheter is connected to a pump that delivers the medication continuously or intermittently, depending on the patient’s needs.
Types of Epidural Injections
- Labor Epidurals: Used to provide pain relief during childbirth by administering a combination of local anesthetics and opioids through a catheter. This allows for a flexible and adjustable pain management approach, accommodating the different stages of labor.
- Epidural Steroid Injections: Utilized to manage chronic pain conditions like sciatica, spinal stenosis, and herniated discs. These injections reduce inflammation and pain by delivering steroids directly to the affected area. The steroids work by reducing inflammation and swelling, which in turn alleviates pressure on the nerves.
- Postoperative Epidurals: After major surgeries, epidurals can provide extended pain relief, reducing the need for systemic opioids and minimizing their side effects. This can lead to improved recovery outcomes and shorter hospital stays.
Benefits of Epidural Administration
Epidural analgesia offers numerous benefits, including:
- Effective Pain Control: Epidurals win for lower body pain! Studies show they offer better relief than strong opioids, especially for surgeries on the lower belly and legs. This enhances patient comfort and facilitates early mobilization post-surgery.
- Reduced Opioid Consumption: Epidurals target pain locally! This reduces reliance on strong opioids, meaning less nausea, vomiting, and trouble breathing.
- Improved Recovery Outcomes: Epidurals boost recovery! Studies show patients experience fewer complications, shorter hospital stays, and a faster return to their normal lives.
- Enhanced Safety: Epidurals offer surprising benefits! Epidurals help high-risk surgery patients breathe easier, fight infection, and avoid heart attacks.
Risks and Complications
While generally safe, epidural administration carries potential risks and complications, such as:
- Minor Complications: These include low blood pressure, headaches, itchy skin, and difficulty urinating. These side effects are usually temporary and manageable with appropriate interventions.
- Serious Complications: Though rare, serious complications can occur, including blood clots, infections, nerve damage, and spinal headaches. Nerve damage is extremely rare and is typically temporary if it occurs. Leakage from the spine can cause bad headaches! An epidural blood patch can fix this problem and ease the pain.
- Drug Reactions: Epidural allergies are rare, but possible. Reactions can occur to the anesthetic or opioids used. Immediate medical attention is required to manage these reactions effectively.
Managing Complications
Effective management of epidural complications involves:
- Monitoring and Supportive Care: Close monitoring of the patient’s vital signs and symptoms during and after the procedure helps detect and manage complications promptly.
- Epidural Blood Patch: For spinal headaches, an epidural blood patch is an effective treatment. This involves injecting a small amount of the patient’s blood into the epidural space to seal any leaks and alleviate headache symptoms.
- Infection Control: Strict aseptic techniques during the procedure and appropriate antibiotic therapy if infections occur can prevent and manage epidural-related infections.
- Patient Education: Informing patients about the signs and symptoms of potential complications and advising them to seek immediate medical attention if they experience any concerning symptoms is crucial for timely intervention.
Post-Procedure Care
Post-epidural care involves:
- Monitoring Recovery: The patient is monitored until the anesthetic effects wear off completely. This includes checking vital signs, pain levels, and motor function to ensure there are no lingering effects or complications.
- Activity Restrictions: Patients are advised against driving or engaging in strenuous activities for at least 24 hours post-procedure to prevent accidents and ensure full recovery.
- Pain Management: Providing additional pain relief measures as needed and ensuring the patient has a clear plan for managing pain at home. This may include oral pain medications, rest, and follow-up appointments to monitor recovery.
- Catheter Care: If an epidural catheter is left in place for continuous medication administration, proper care and hygiene must be maintained to prevent infections. Patients should be instructed on how to care for the catheter site and what signs of infection to watch for.
Advances in Epidural Administration
Recent advances in epidural administration focus on improving safety, efficacy, and patient comfort. Innovations include:
- Ultrasound Guidance: The use of ultrasound imaging to guide needle and catheter placement has improved the accuracy and safety of epidural procedures. This technique allows for real-time visualization of the anatomy and reduces the risk of complications.
- Patient-Controlled Epidural Analgesia (PCEA): PCEA systems allow patients to self-administer controlled doses of epidural medication through a pump, providing personalized pain management and increasing patient satisfaction. This method is particularly useful in labor and postoperative settings.
- New Drug Formulations: Advances in pharmacology have led to the development of new local anesthetics and opioid formulations with improved safety profiles and longer durations of action. These innovations enhance the effectiveness of epidural analgesia while minimizing side effects.
Clinical Studies and Research
Ongoing research continues to explore the benefits and risks of epidural administration. Clinical studies have demonstrated the efficacy of epidurals in various settings, from labor and delivery to postoperative pain management and chronic pain conditions. Key findings include:
- Labor and Delivery: Studies have shown that epidural anesthesia significantly reduces pain during childbirth without increasing the risk of cesarean delivery. Women who receive epidurals report higher satisfaction with their childbirth experience compared to those who use other pain relief methods. Research also indicates that epidurals do not negatively impact breastfeeding success or neonatal outcomes (Pain Management Education at UCSF) (American Pregnancy Association).
- Postoperative Pain Management: Epidural anesthesia shines in major surgery! Research shows patients experience better pain control after abdominal or chest procedures when they receive epidurals. This also translates to needing fewer opioid painkillers after surgery. This can lead to enhanced recovery, shorter hospital stays, and decreased incidence of chronic postoperative pain (Wikipedia) (Spine-health).
- Chronic Pain Management: Epidural steroid injections fight chronic pain! They bring relief to conditions like lumbar radiculopathy and spinal stenosis. Studies suggest that these injections can reduce pain and improve function, although the duration of relief varies among individuals (American Pregnancy Association) (Pain Management Education at UCSF).
Future Directions and Innovations
The future of epidural administration is likely to see continued advancements in technology, drug formulations, and procedural techniques. Areas of focus include:
- Enhanced Imaging Techniques: Advanced imaging steps up! 3D ultrasound & MRI may guide epidural needles for better placement. New Tech Makes Epidurals Safer! Advancements boost accuracy and safety of these pain rocedures (American Pregnancy Association) (Pain Management Education at UCSF).
- Biodegradable Drug Delivery Systems: Researchers are investigating the development of biodegradable drug delivery systems for epidural use.
- New pain relief systems: Offer long-lasting drugs, ditch the catheter, and cut infection risks!
- (Pain Management Education at UCSF) (Spine-health).
- Personalized Medicine: Future epidurals: Customized pain relief! Genetics will guide medication choice for each patient. This could enhance the effectiveness and safety of epidural anesthesia (Pain Management Education at UCSF) (nhs.uk).
- Combination Therapies: Researchers are exploring ways to improve epidural pain relief. They’re studying combinations of medications like non-opioid painkillers, anti-inflammatory drugs, and nerve signal regulators. These combination therapies might be a game-changer for pain management. New epidurals aim for stronger relief, fewer side effects. No more heavy reliance on opioids! (Wikipedia) (Yale Medicine).
Conclusion
Even though new approaches are being explored, epidural administration is still a vital tool for pain management. It offers excellent pain relief, keeps patients comfortable, and helps them recover faster across various medical situations. Epidural administration remains a cornerstone of pain management, offering significant benefits for pain relief, patient comfort, and recovery. While some risks exist, advancements in technology, drug formulations, and techniques are continuously improving its safety and effectiveness. Researchers are even exploring combination therapies to potentially achieve even stronger pain relief with fewer side effects. The future of epidural anesthesia is bright! Epidural anesthesia is getting better! Thanks to ongoing research, it’s finding new applications and becoming even more effective at managing pain and helping patients heal.
The history and development of epidural anesthesia highlight the importance of continual medical research and adaptation. Epidural administration has come a long way. Once an experiment, it’s now a routine procedure in surgery and childbirth, showcasing medical advancements and improved patient care. The future of epidurals is exciting! New tech and personalized care are on the horizon, promising to make this pain-relief method even more powerful and integrated into modern medicine.