- Liver Cancer and Obesity: An In-Depth Analysis
- Understanding Liver Cancer
- Obesity and Liver Cancer: A Growing Concern
- Obesity Overtakes Smoking and Alcohol as Leading Cause of Liver Cancer
- Risk Factors Associated with Obesity and Liver Cancer
- Preventive Measures and Lifestyle Changes
- The Role of Public Health Initiatives
- Latest Research Findings
- Conclusion
Liver Cancer and Obesity: An In-Depth Analysis
Liver cancer, primarily hepatocellular carcinoma (HCC), is a serious health concern globally. Recent research highlights a significant shift in risk factors, with obesity overtaking smoking and alcohol consumption as a leading cause of liver cancer. This article explores the intricate relationship between liver cancer and obesity, examining the mechanisms, risk factors, preventive measures, and the latest research findings.
Understanding Liver Cancer
Liver cancer is a type of cancer that begins in the liver cells. It is the sixth most common cancer worldwide and the second leading cause of cancer-related deaths. There are several types of liver cancer, with hepatocellular carcinoma (HCC) being the most common. Other types include intrahepatic cholangiocarcinoma and hepatoblastoma.
Types of Liver Cancer
- Hepatocellular Carcinoma (HCC): The most prevalent type, accounting for approximately 75% of liver cancer cases. It starts in the hepatocytes, the main type of liver cell.
- Intrahepatic Cholangiocarcinoma: Also known as bile duct cancer, it originates in the bile ducts within the liver.
- Hepatoblastoma: A rare type that usually affects children under the age of three.
- Angiosarcoma: A rare cancer that begins in the blood vessels of the liver.
Obesity and Liver Cancer: A Growing Concern
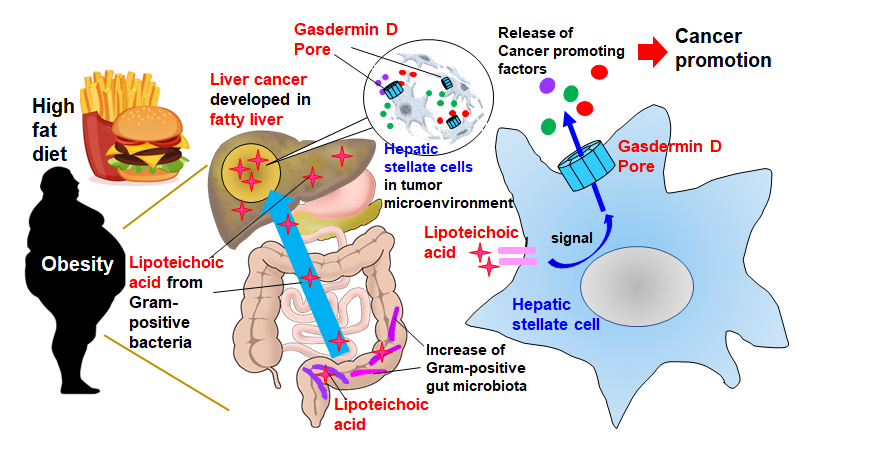
Obesity is characterized by an excessive accumulation of body fat. It is now recognized as a significant risk factor for various health issues, including liver cancer. The relationship between obesity and liver cancer is supported by numerous studies, indicating that obesity can lead to the development of non-alcoholic fatty liver disease (NAFLD), which can progress to non-alcoholic steatohepatitis (NASH), cirrhosis, and ultimately, liver cancer【8†source】【10†source】.
Mechanisms Behind the Link
- Insulin Resistance and Inflammation: Obesity often results in insulin resistance, which leads to higher insulin and glucose levels in the blood. This condition promotes chronic inflammation, damaging liver cells and contributing to cancer development【10†source】.
- Fat Accumulation in the Liver: Excess fat storage in the liver, a hallmark of NAFLD, causes liver inflammation and fibrosis. This can progress to NASH and cirrhosis, significantly increasing the risk of liver cancer【8†source】.
- Hormonal Changes: Obesity alters the levels of certain hormones, such as leptin and adiponectin, which regulate inflammation and cell proliferation. These hormonal changes create an environment conducive to cancer development【11†source】.
Obesity Overtakes Smoking and Alcohol as Leading Cause of Liver Cancer
Historically, liver cancer was predominantly associated with chronic hepatitis B and C infections, excessive alcohol consumption, and smoking. However, recent research indicates that obesity has surpassed these factors as the leading cause of liver cancer. This shift underscores the growing epidemic of obesity and its profound impact on public health【8†source】【9†source】.
Comparative Risk Analysis
- Alcohol and Smoking: While alcohol consumption and smoking remain significant risk factors for liver cancer, their relative impact has diminished compared to obesity. Alcohol can cause direct liver damage, leading to cirrhosis and liver cancer. Smoking introduces carcinogens that can affect liver cells and contribute to cancer development.
- Obesity’s Increasing Impact: The rise in obesity rates has paralleled an increase in NAFLD and NASH cases. These conditions are now recognized as major precursors to liver cancer, with obesity-induced metabolic changes playing a critical role in liver carcinogenesis【8†source】.
Risk Factors Associated with Obesity and Liver Cancer
- Type 2 Diabetes: Obesity is a major risk factor for type 2 diabetes, which is also linked to an increased risk of liver cancer. Diabetic patients often have higher insulin levels, contributing to liver cell proliferation and cancer risk【10†source】.
- Chronic Inflammation: Persistent inflammation in obese individuals leads to liver cell damage and increases the likelihood of liver cancer. Inflammatory cytokines produced by adipose tissue play a crucial role in this process【11†source】.
- Genetic Predispositions: Certain genetic factors may predispose obese individuals to develop liver cancer. Studies are ongoing to identify specific genetic markers associated with increased risk【7†source】.
- Non-Alcoholic Fatty Liver Disease (NAFLD): NAFLD is strongly associated with obesity and can progress to NASH, cirrhosis, and liver cancer. The accumulation of fat in liver cells leads to inflammation and fibrosis, creating a fertile ground for cancer development【10†source】.
Preventive Measures and Lifestyle Changes
- Maintaining a Healthy Weight: Achieving and maintaining a healthy weight through a balanced diet and regular physical activity is crucial. Reducing body fat decreases the risk of developing NAFLD and subsequent liver complications【9†source】【11†source】.
- Dietary Adjustments: Consuming a diet rich in fruits, vegetables, whole grains, and lean proteins can help manage weight and reduce liver cancer risk. Limiting alcohol intake is also essential, as alcohol can exacerbate liver damage【8†source】.
- Regular Screening: For individuals with obesity and other risk factors, regular screening for liver disease is vital. Early detection of NAFLD or NASH can lead to timely interventions and reduce the risk of progression to liver cancer【7†source】.
- Physical Activity: Engaging in regular physical exercise helps in maintaining a healthy weight, improving insulin sensitivity, and reducing inflammation. Exercise is a powerful tool in preventing obesity-related liver cancer【9†source】.
- Medications and Supplements: Certain medications and dietary supplements, such as metformin for diabetes and milk thistle for liver health, may help manage obesity-related conditions and reduce liver cancer risk【10†source】.
The Role of Public Health Initiatives
Public health initiatives play a crucial role in addressing the obesity epidemic and reducing liver cancer risk. These initiatives include:
- Education and Awareness Campaigns: Increasing public awareness about the risks of obesity and its link to liver cancer through education campaigns.
- Community Programs: Implementing community-based programs that promote healthy eating and physical activity, particularly in high-risk populations【9†source】【11†source】.
- Policy Changes: Advocating for policy changes that support healthy lifestyles, such as regulations on food labeling, taxation of sugary drinks, and improved access to healthy foods and recreational facilities【8†source】.
- Healthcare Provider Involvement: Encouraging healthcare providers to screen for obesity and related conditions, provide dietary and lifestyle counseling, and refer patients to appropriate weight management programs【11†source】.
Latest Research Findings
Recent studies continue to shed light on the connection between obesity and liver cancer. Key findings include:
- Coffee Consumption: Research suggests that coffee consumption may have a protective effect against liver cancer. Coffee contains compounds that can enhance liver function and reduce inflammation【8†source】.
- Physical Activity: Studies indicate that regular physical activity can significantly reduce the risk of liver cancer by improving insulin sensitivity and reducing inflammation【9†source】.
- Dietary Patterns: Eating a diet rich in fiber, fruits, and vegetables may lower your risk of liver cancer. Conversely, diets high in processed foods, sugars, and unhealthy fats increase the risk【8†source】.
- Genetic Research: Ongoing genetic research aims to identify specific genes associated with increased liver cancer risk in obese individuals. Understanding these genetic factors could lead to targeted prevention and treatment strategies【7†source】.
Conclusion
The relationship between liver cancer and obesity is complex and multifaceted. Obesity significantly increases the risk of liver cancer through mechanisms involving insulin resistance, inflammation, and fat accumulation in the liver. The shift in liver cancer risk factors, with obesity now surpassing smoking and alcohol consumption, highlights the urgent need for effective public health strategies to combat obesity. Maintaining a healthy weight through diet, exercise, and lifestyle changes is crucial in reducing liver cancer risk. Continued research and public health initiatives are essential to address this growing health concern and improve outcomes for those at risk.
For more information on liver cancer and obesity, visit the American Cancer Society, the American Institute for Cancer Research, and the Centers for Disease Control and Prevention.

From what I’ve learned in uni the increased rate of cancer in obese people is more due to increased inflammation and release of molecules that stimulate cancer growth. The number of cells do play a role in the risk, but a minor one so the effects should be slight if even measurable.
From what I’ve learned in uni the increased rate of cancer in obese people is more due to increased inflammation and release of molecules that stimulate cancer growth. The number of cells do play a role in the risk, but a minor one so the effects should be slight if even measurable.
Obesity or being very overweight causes a lot of issues and we take medication that puts a lot of pressure on the liver.
If we could get people to lose weight I am sure it would lower all ilnesses.
I was sitting on the floor playing the PS4. Paused the game and went to stand up to go to the bathroom, and I realized that it had become a real effort to stand up.
While in the bathroom, standing there doing my thing, I idly realized that my then-14YO daughter was the same age I was when my own father died. He died of everything cancer due to smoking. He loved smoking so much that he continued to smoke even after having most of his jaw, tongue, throat, lungs, and liver removed. I always thought that was the absolute pinnacle of idiocy…and then I realized that I was doing the same thing, eating myself into a grave. I knew I was fat yet continued my unhealthy lifestyle. I was my father — but I wasn’t gonna turn my daughter into me.
The next day I made a doctor’s appointment for a check up. In the meantime I started purging the kitchen of junk food and reading up on sustainable weight loss techniques. I got the “Lose It” app for calorie counting (which really was instrumental for me). I came up with a plan and ran it past my doctor, who was in general agreement.
I weighed in at 287 lbs. About 9-10 months later I weighed in at 186, but it was very difficult for me to sustain it. Eventually I settled into around 200-205 which is comfortable for me, and I am sustaining it pretty easily.
And my daughter, now 16, still has a dad.
Getting told I might have cancer. I worked my butt off and lost 80 pounds. It turned out to be benign, but I never looked back and am healthier and look better at 49 than I did even in my 20s.