- AI Better Predicts Back Surgery Outcomes: Innovations
- Introduction
- Composition and Capabilities of AI in Back Surgery
- Mechanisms of Action
- Scientific Evidence on Efficacy
- Safety and Operational Guidelines
- Alternative Treatments and Technologies
- Case Studies and Patient Testimonials
- Future Directions and Research
- Conclusion
- References
- Recommended External Links
- Recommended Internal Links
AI Better Predicts Back Surgery Outcomes: Innovations
Introduction
Artificial Intelligence (AI) is revolutionizing the medical field, particularly in predicting outcomes for back surgeries. By analyzing vast amounts of patient data, AI can forecast recovery trajectories, potential complications, and overall success rates of surgeries with unprecedented accuracy. This article delves into the role of AI in back surgery, exploring its mechanisms, scientific evidence, safety, and potential future directions.
Composition and Capabilities of AI in Back Surgery
Key Algorithms and Their Roles
- Predictive Analytics: AI algorithms use historical patient data to predict outcomes. These include factors like age, medical history, type of surgery, and pre-existing conditions. Predictive analytics helps surgeons to anticipate and mitigate risks, ultimately improving patient outcomes.
- Machine Learning Models: Models such as neural networks and decision trees analyze complex datasets to identify patterns that can predict surgical success and potential complications. These models continuously learn and adapt, becoming more accurate over time as they process more data.
- Natural Language Processing (NLP): NLP tools extract useful information from unstructured data like medical notes and patient histories, enhancing predictive accuracy. By analyzing free-text data, NLP can uncover insights that structured data alone might miss, providing a more comprehensive understanding of patient health.
Mechanisms of Action
How AI Predicts Back Surgery Outcomes
- Data Integration: AI integrates data from various sources, including electronic health records (EHRs), imaging studies, and patient questionnaires. This holistic approach ensures that all relevant information is considered in the prediction process.
- Pattern Recognition: AI systems identify patterns and correlations that are not apparent to human analysts, providing insights into factors that affect surgical outcomes. For example, AI might detect that certain combinations of pre-existing conditions increase the risk of post-surgical complications.
- Continuous Learning: AI models continuously improve by learning from new data, making them more accurate over time. This ability to evolve with each new piece of information is a key advantage of AI over traditional predictive methods.
Role of AI in Enhancing Decision-Making
AI assists surgeons by providing data-driven insights that can influence pre-surgical planning and post-surgical care. This includes:
- Risk Stratification: Identifying patients at higher risk of complications to tailor preoperative and postoperative interventions. This allows for more personalized and effective treatment plans.
- Customized Treatment Plans: Suggesting personalized treatment plans based on predicted outcomes. By tailoring care to individual patients’ needs, AI can improve both the effectiveness and efficiency of medical interventions.
Scientific Evidence on Efficacy
Overview of Studies Conducted
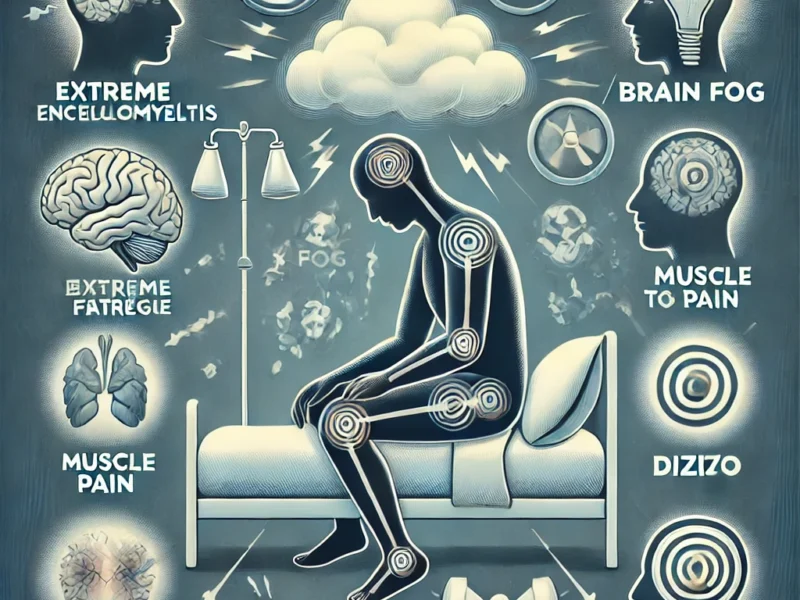
Recent studies have demonstrated the efficacy of AI in predicting back surgery outcomes. For instance, research from Cedars-Sinai showed that AI algorithms could accurately predict which patients would have successful pain management post-surgery. Other studies have found that AI can reduce readmission rates and improve recovery times by identifying patients who need additional care.
Analysis of Results and Their Significance
Results from these studies indicate that AI can significantly enhance the accuracy of outcome predictions, leading to better patient management and optimized surgical results. Patients identified as high-risk can receive targeted interventions, reducing the likelihood of complications and improving overall outcomes. The significance of these findings lies in AI’s potential to transform how surgeons approach back surgery, shifting from a one-size-fits-all approach to a more personalized, data-driven model of care.
Limitations of Current Research
Despite promising results, there are limitations:
- Data Quality: The accuracy of AI predictions depends on the quality and comprehensiveness of the data. Incomplete or biased data can lead to inaccurate predictions.
- Generalizability: Models trained on specific datasets may not perform well across different populations or healthcare settings. Ensuring that AI models are robust and applicable to diverse patient groups is an ongoing challenge.
Safety and Operational Guidelines
Recommended Dosages for AI Utilization
AI tools in healthcare should be used under strict protocols to ensure patient safety. Recommendations include:
- Validation: AI models must be rigorously validated in clinical settings before widespread use. This involves extensive testing and verification to ensure that the models perform as expected in real-world scenarios.
- Continuous Monitoring: Regular updates and monitoring of AI systems to maintain their accuracy and reliability. This includes tracking the performance of AI models and making adjustments as needed to address any issues that arise.
Potential Side Effects and Contraindications
While AI offers many benefits, potential risks include:
- Bias: AI models can perpetuate existing biases in healthcare data, leading to unequal treatment outcomes. Addressing these biases is crucial to ensure that AI benefits all patients equally.
- Overreliance: Overreliance on AI predictions without human oversight can lead to suboptimal clinical decisions. It is essential to maintain a balance between AI-driven insights and clinical judgment.
Alternative Treatments and Technologies
Comparison with Other Predictive Tools
- Traditional Statistical Models: Compared to AI, traditional models analyze fewer variables and may miss complex interactions between factors. AI’s ability to process large, complex datasets gives it a distinct advantage.
- Clinical Judgment: While expert judgment is invaluable, AI can augment decision-making by providing data-driven insights that are not immediately apparent to clinicians. This can enhance the overall quality of care.
Emerging Technologies in Back Surgery
Innovations such as augmented reality (AR) and virtual reality (VR) are enhancing surgical training and precision, contributing to improved outcomes. These technologies allow surgeons to practice and refine their techniques in a risk-free environment, leading to better surgical performance. Additionally, telehealth services enable better pre- and post-operative care, ensuring continuous patient support.
Case Studies and Patient Testimonials
Personal Experiences with AI-Enhanced Surgeries
Patients who underwent AI-assisted back surgeries have reported higher satisfaction rates due to personalized care plans and better pain management. Testimonials highlight the role of AI in predicting and mitigating post-surgical complications. These personal stories underscore the real-world impact of AI on patient outcomes.
Case Studies Highlighting AI Impact
Case studies from leading medical centers show that AI can reduce readmission rates and improve recovery times. These studies underscore the potential of AI to transform back surgery outcomes by providing tailored interventions based on predictive analytics. For example, one case study might detail how an AI model identified a high-risk patient who was then given additional preoperative care, resulting in a smoother recovery.
Future Directions and Research
Potential Areas for Further Exploration
Future research could focus on:
- Expanding Data Sources: Integrating more diverse datasets to improve model generalizability. This might include data from different geographic regions, healthcare systems, and patient demographics.
- Refining Algorithms: Developing more sophisticated algorithms to enhance predictive accuracy. Advances in machine learning techniques could lead to even more precise predictions.
The Role of Technology in Advancing AI Research
Advancements in computing power, data storage, and machine learning techniques will continue to drive AI innovation in healthcare. These technologies will enable more accurate and comprehensive analyses, leading to better patient outcomes. The integration of AI with other emerging technologies, such as genomics and personalized medicine, holds promise for even more groundbreaking discoveries.
Conclusion
Summary of Findings
AI is transforming back surgery by providing accurate predictions of surgical outcomes. These advancements lead to better preoperative planning, personalized postoperative care, and overall improved patient satisfaction. However, continuous research and ethical considerations are essential to fully harness AI’s potential in healthcare.
Balancing Scientific Evidence and Clinical Practice
While AI offers significant benefits, it should complement, not replace, clinical judgment. Integrating AI into clinical workflows requires careful consideration of ethical implications and continuous validation. The goal is to enhance, not overshadow, the expertise of healthcare professionals.
Final Thoughts
AI holds great promise in enhancing the accuracy and outcomes of back surgeries. As technology continues to evolve, the hope for more precise and personalized medical interventions grows, offering new avenues for improving patient care. By embracing AI, the future of back surgery looks promising, with the potential for more accurate predictions, personalized treatments, and improved patient outcomes.
References
- Cedars-Sinai Department of Computational Biomedicine. “The Human Side of AI: Predicting Spine Surgery Outcomes” Cedars-Sinai Blog.
- The Healthcare Guys. “Is Technology Transforming Back Surgery Outcomes for the Better?” The Healthcare Guys.
- National Institutes of Health (NIH). “Artificial Intelligence in Healthcare: The Future of Medicine” NIH.
Recommended External Links
- How AI is Revolutionizing Healthcare – Explore the broader impact of AI on healthcare.
- Innovations in Medical Technology – Discover the latest advancements in medical technology.
- The Role of AI in Modern Medicine – Learn about the scientific foundation and future prospects of AI in medicine.
Recommended Internal Links
AI Improves Prediction of Back Surgery Outcomes
By embracing AI, the future of back surgery looks promising, with the potential for more accurate predictions, personalized treatments, and improved patient outcomes.

Hope the AI is more intelligent than the doctors.
With all the things I see AI accomplish, I’ll be impressed if A.I. can be taught to read doctors handwriting. 😂
Hello everyone,
I’m currently exploring the feasibility of a project I’m planning to undertake and would greatly appreciate any insights or advice from this community.
**Background:** I’m a neurosurgeon in my final year of residency, specializing in spine surgery. I believe that AI has significant potential in this field. Typically, when dealing with spine pathologies identified through imaging and symptoms, there are multiple surgical approaches available. These approaches vary widely in cost and can lead to different outcomes, both short-term and long-term. Surprisingly, the spine surgery literature has yet to reach a strong consensus on the optimal approaches for even straightforward cases.
**My Objective:** Simply put, I want to use machine learning to analyze pre-operative patient data and imaging (such as MRIs, CTs, and X-rays) along with post-operative outcomes and imaging to develop predictive models that can:
1. Predict the type of surgical intervention that will yield the best outcome for a new patient based on their pre-operative data, symptoms, and imaging.
2. Provide surgeons with the optimal spinal correction parameters to implement during surgery, such as the precise degrees of curvature correction needed.
Over the past year, I’ve worked closely with hospital administrators and the radiology department to establish a pathway for accessing over 2,500 patient imaging records and associated data. This has all been approved by our institutional review board, ensuring that all data is HIPAA compliant and de-identified. Additionally, I’ve partnered with a statewide spine surgery outcomes database, which collects detailed pre-and post-op data from major centers. My institutional data can be cross-referenced with this statewide data to enhance outcomes analysis.
While I lack the technical expertise in computer science and machine learning to assess the feasibility of developing and training ML algorithms on these datasets, I understand that this is a large-scale endeavor that will require substantial resources. Fortunately, through networking, I’ve secured a pledge of $3 million from a prominent local financier with strong ties to our hospital system. This investment is contingent on my ability to assemble a technical team. I also have meetings lined up with other interested investors, with a goal of raising about $5 million in total. My proposal to the hospital, which they fully support, involves establishing a company with the hospital as an equity partner. In return, the hospital will facilitate streamlined access to patient and imaging data. The company will be structured to allow for external funding through venture investments.
The tools developed through this initiative could have significant commercial potential in the spine surgery market and, more importantly, could greatly improve surgical outcomes for patients.
Of course, none of this can move forward without a technical team in place. But first, I’m hoping to discuss the technical feasibility of a project like this, as well as the types and amounts of resources that would be needed.
I’ve kept this post concise for brevity, but I’m happy to provide more details in the comments if needed.